Dry eczema, also known as xerotic eczema or asteatotic eczema, is a chronic skin condition characterized by dry, itchy, and inflamed patches of skin. It commonly affects individuals with a history of atopic dermatitis or those with sensitive skin. Understanding the causes, symptoms, and treatment options is crucial for effectively managing this condition and improving quality of life.
Definition of Dry Eczema and Its Causes
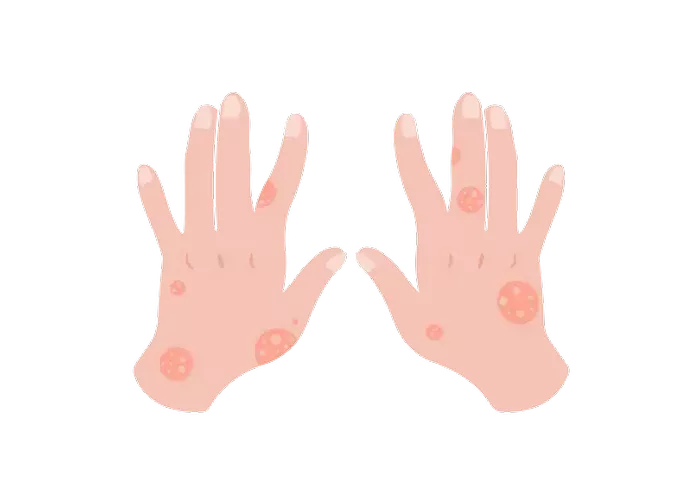
Dry eczema is a type of eczema characterized by severely dry, cracked, and scaly skin. It often appears on the arms, legs, hands, and feet but can occur anywhere on the body. The exact cause of dry eczema is not fully understood, but several factors contribute to its development:
1. Impaired Skin Barrier: Individuals with dry eczema often have a compromised skin barrier, allowing moisture to escape and irritants to penetrate the skin more easily.
2. Genetics: Genetics play a significant role in predisposing individuals to eczema. People with a family history of eczema or other allergic conditions are more likely to develop dry eczema.
3. Environmental Factors: Exposure to harsh weather conditions, such as cold, dry air in winter, or excessive heat and humidity in summer, can exacerbate dry eczema symptoms.
4. Skin Sensitivity: Individuals with sensitive skin are more prone to developing eczema. Factors such as certain fabrics, soaps, detergents, and skincare products can trigger flare-ups.
Common Symptoms of Dry Eczema
The symptoms of dry eczema can vary in severity but commonly include:
Dryness: The affected skin is often dry, rough, and scaly to the touch.
Itchiness: Intense itching is a hallmark symptom of dry eczema, leading to scratching and further skin damage.
Redness: The affected areas may appear red or inflamed, especially during flare-ups.
Cracking and Peeling: The skin may crack, peel, or develop fissures, making it vulnerable to infections.
Bleeding: In severe cases, scratching or dryness can cause the skin to bleed.
Overview of Treatment Options
Managing dry eczema involves a multifaceted approach aimed at hydrating the skin, reducing inflammation, and preventing flare-ups. Treatment options can be categorized into topical, systemic, and home remedies.
1. Topical Treatments:
- Moisturizers: Emollients and moisturizing creams help hydrate the skin and repair the skin barrier. Look for products containing ceramides, hyaluronic acid, or colloidal oatmeal.
- Topical Corticosteroids: Prescription or over-the-counter corticosteroid creams can reduce inflammation and itching during flare-ups. Use them sparingly and under the guidance of a healthcare professional to avoid side effects.
- Topical Calcineurin Inhibitors: These medications, such as tacrolimus and pimecrolimus, are often used as alternatives to corticosteroids for long-term management of eczema.
- Barrier Repair Creams: Formulated with ingredients like petrolatum or dimethicone, barrier repair creams help protect and repair the skin barrier.
2. Systemic Treatments:
- Oral Antihistamines: These medications can help alleviate itching and improve sleep quality, particularly when itching disrupts sleep.
- Oral Corticosteroids: In severe cases of eczema, short courses of oral corticosteroids may be prescribed to quickly reduce inflammation. However, long-term use is not recommended due to potential side effects.
- Immunosuppressants: Drugs like cyclosporine or methotrexate may be prescribed for individuals with severe, refractory eczema that does not respond to other treatments.
3. Home Remedies:
- Oatmeal Baths: Adding colloidal oatmeal to lukewarm bathwater can help soothe itchy skin and reduce inflammation.
- Coconut Oil: Applying virgin coconut oil to the affected areas can provide moisture and anti-inflammatory benefits.
- Wet Wrap Therapy: This involves applying a damp layer of clothing or bandages over moisturized skin to enhance hydration and reduce itching.
Factors to Consider When Choosing a Treatment
When selecting a treatment for dry eczema, several factors should be considered:
1. Severity of Symptoms: The severity of eczema symptoms will influence the choice of treatment. Mild cases may only require emollients and moisturizers, while more severe cases may necessitate prescription medications.
2. Skin Sensitivity: Individuals with sensitive skin should opt for fragrance-free, hypoallergenic products to minimize the risk of irritation.
3. Medical History: Patients with pre-existing medical conditions or taking other medications should consult with a healthcare professional before starting new treatments to avoid potential drug interactions or exacerbation of underlying conditions.
Step-by-Step Instructions for Using Different Treatments
1. Topical Treatments:
- Apply a liberal amount of moisturizer to clean, dry skin at least twice daily, paying special attention to areas prone to dryness.
- Use topical corticosteroids as directed by a healthcare professional, applying a thin layer to affected areas and gently rubbing it in until absorbed.
- Follow the prescribed regimen for topical calcineurin inhibitors, applying a thin layer to affected areas and avoiding prolonged sun exposure.
2. Oral Medications:
- Take oral antihistamines as directed, typically before bedtime to alleviate itching and improve sleep quality.
- Follow the prescribed dosage and duration for oral corticosteroids or immunosuppressants, and attend regular follow-up appointments with a healthcare provider to monitor for side effects.
3. Home Remedies:
- Add one cup of colloidal oatmeal to a warm bath and soak for 10-15 minutes. Pat skin dry gently afterward and apply moisturizer.
- Apply virgin coconut oil to affected areas as needed, especially after bathing when the skin is still damp.
- Consult with a healthcare professional before attempting wet wrap therapy to ensure proper technique and safety.
Product Recommendations
While specific product recommendations may vary based on individual preferences and sensitivities, some widely recommended brands for eczema management include:
- Moisturizers: CeraVe, Eucerin, Aveeno, Cetaphil
- Topical Corticosteroids: Hydrocortisone cream, Triamcinolone cream
- Topical Calcineurin Inhibitors: Protopic (tacrolimus), Elidel (pimecrolimus)
- Barrier Repair Creams: Aquaphor, Vanicream, Cetaphil Restoraderm
Tips for Managing Eczema Flare-Ups
1. Avoid Triggers: Identify and avoid triggers that exacerbate eczema symptoms, such as harsh soaps, allergens, and environmental factors.
2. Maintain Skin Hydration: Moisturize regularly with emollients and avoid prolonged exposure to hot water, which can strip the skin of natural oils.
3. Practice Gentle Skincare: Use mild, fragrance-free skincare products and avoid scrubbing or rubbing the skin vigorously.
4. Manage Stress: Stress can worsen eczema symptoms, so practice stress-reducing techniques such as mindfulness, meditation, or yoga.
5. Seek Medical Advice: Consult with a doctor or dermatologist if eczema symptoms persist or worsen despite home treatments, as they may recommend alternative therapies or adjustments to the treatment regimen.
Importance of Consulting a Doctor or Dermatologist
While many cases of dry eczema can be effectively managed with over-the-counter treatments and home remedies, it’s essential to consult with a healthcare professional, particularly for severe or persistent symptoms. A dermatologist can provide personalized treatment recommendations based on the individual’s medical history, skin type, and specific needs. Additionally, they can monitor for potential side effects of long-term treatments and adjust the treatment plan accordingly.
Conclusion
In conclusion, managing dry eczema requires a comprehensive approach that addresses both symptom relief and long-term skin health. By understanding the causes, symptoms, and treatment options for dry eczema, individuals can take proactive steps to manage their condition effectively and improve their quality of life. Always consult with a healthcare professional for personalized advice and guidance tailored to your unique needs and circumstances.