Hidradenitis Suppurativa (HS) and Lupus are two distinct medical conditions that can significantly impact an individual’s quality of life. While they affect different systems of the body and have unique pathophysiologies, there has been speculation about a potential association between the two. In this article, we delve into the definitions, pathophysiologies, prevalence, and demographics of both HS and Lupus, address the existing research on their potential link, differentiate their symptoms, and discuss treatment and management strategies.
Defining HS and Lupus
1. Hidradenitis Suppurativa (HS):
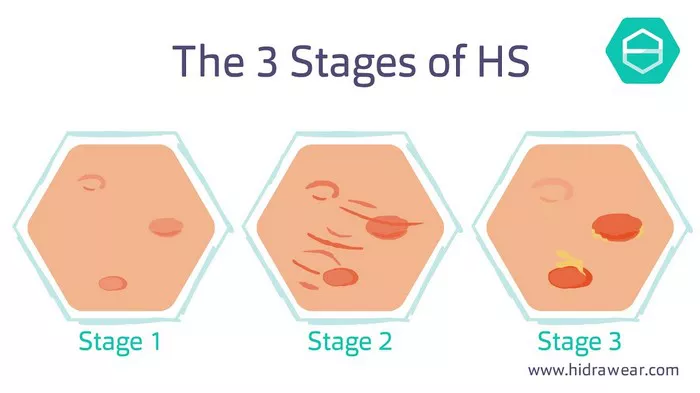
Hidradenitis Suppurativa, also known as acne inversa, is a chronic inflammatory skin condition characterized by painful, recurrent nodules, abscesses, and sinus tracts primarily affecting areas rich in apocrine glands, such as the axillae, groin, and buttocks. The exact cause of HS remains unclear, but it is believed to involve a combination of genetic, hormonal, and environmental factors. The condition often leads to significant morbidity and can profoundly impact patients’ physical and emotional well-being.
2. Lupus:
Lupus, or systemic lupus erythematosus (SLE), is a complex autoimmune disease that can affect multiple organs and systems in the body, including the skin, joints, kidneys, and cardiovascular system. Lupus is characterized by the production of autoantibodies that target various components of the body’s own cells and tissues, leading to inflammation, tissue damage, and a wide range of symptoms. While the precise cause of lupus remains elusive, it is thought to involve a combination of genetic predisposition, environmental triggers, and dysregulation of the immune system.
3. Prevalence and Demographics:
Hidradenitis Suppurativa typically begins after puberty and affects approximately 1-4% of the population, with a higher prevalence among women and individuals of African descent. Lupus, on the other hand, predominantly affects women of childbearing age, with an estimated prevalence of 20-150 cases per 100,000 individuals. Lupus also disproportionately affects certain racial and ethnic groups, including African Americans, Hispanics, and Asians.
Addressing the Link Between HS and Lupus
While there is some research suggesting a potential association between HS and Lupus, the nature of this relationship remains unclear. Several studies have reported an increased prevalence of autoimmune diseases, including Lupus, among patients with HS, suggesting a possible shared genetic or immunological predisposition. Additionally, both conditions are characterized by chronic inflammation and dysregulation of the immune system, leading to speculation that they may share common pathophysiological mechanisms.
However, it is essential to note that the evidence linking HS and Lupus is largely observational and correlational, and causality has not been established. Further research, including longitudinal studies and mechanistic investigations, is needed to elucidate the nature of this potential association fully. In the meantime, individuals experiencing symptoms of either HS or Lupus should seek medical evaluation and appropriate management by healthcare professionals familiar with these conditions.
Differentiating HS and Lupus
Comparison Table:
| Aspect | Hidradenitis Suppurativa (HS) | Lupus |
| Affected Areas of Body | Axillae, groin, buttocks, under breasts | Skin, joints, kidneys, cardiovascular system |
| Types of Skin Lesions | Painful nodules, abscesses, sinus tracts | Butterfly rash, discoid lesions, photosensitivity |
| Common Systemic Symptoms | Fatigue, malaise, fever, joint pain | Fatigue, fever, joint pain, organ involvement |
| Diagnostic Criteria | Clinical examination, imaging, biopsy | Clinical and laboratory criteria (e.g., ANA, anti-dsDNA) |
| Treatment Options | Antibiotics, anti-inflammatory medications, surgical excision | Immunosuppressive medications, corticosteroids, lifestyle modifications |
Treatment and Management
1. Hidradenitis Suppurativa:
Treatment for HS aims to reduce inflammation, alleviate symptoms, and prevent disease progression. Options may include topical and systemic antibiotics, anti-inflammatory medications (e.g., corticosteroids, TNF-alpha inhibitors), and surgical interventions (e.g., drainage, excision). Lifestyle modifications such as weight loss, smoking cessation, and avoiding tight clothing may also be beneficial.
2. Lupus:
Management of Lupus typically involves a multidisciplinary approach aimed at controlling inflammation, minimizing organ damage, and improving quality of life. Treatment may include immunosuppressive medications (e.g., hydroxychloroquine, corticosteroids, immunomodulators), lifestyle modifications (e.g., sun protection, regular exercise), and supportive care. Close monitoring by healthcare providers is essential to adjust treatment regimens as needed and address any complications or disease flares.
Conclusion
In conclusion, while there is ongoing speculation about a potential link between Hidradenitis Suppurativa and Lupus, the nature of this association remains to be fully elucidated. Both conditions pose significant challenges for patients and healthcare providers, emphasizing the importance of accurate diagnosis, individualized treatment plans, and ongoing research to improve outcomes and quality of life for affected individuals. If you suspect you may have symptoms of either HS or Lupus, it is crucial to consult with a healthcare professional for proper evaluation and management.