Eczema and asthma are two common chronic inflammatory conditions that affect millions of individuals worldwide. Despite manifesting in different ways—eczema primarily affecting the skin and asthma predominantly impacting the airways—these conditions share more than just symptoms. They often coexist within the same individual or within families, suggesting a significant underlying connection. Understanding the relationship between eczema and asthma is crucial for better management and treatment of both conditions.
The Atopic March: Understanding the Progression of Atopic Conditions
The concept of the “atopic march” refers to the natural progression of allergic diseases from infancy to adulthood. It describes the sequential development of various allergic conditions, often starting with eczema in infancy, followed by asthma and allergic rhinitis later in childhood. While not all individuals follow this exact progression, it provides valuable insight into the interconnected nature of these conditions.
Shared Genetic Predisposition: The Role of Genetics in Eczema and Asthma
Genetic predisposition plays a significant role in the development of both eczema and asthma. Numerous studies have identified specific genetic variations associated with an increased risk of these conditions. Notably, mutations in genes related to skin barrier function, immune response, and inflammation have been implicated in both eczema and asthma.
For instance, filaggrin gene mutations, which compromise the integrity of the skin barrier, are strongly associated with eczema and also linked to an increased risk of asthma. Similarly, variations in genes encoding components of the immune system, such as interleukins and cytokines, contribute to the development of both conditions.
The Immunological Connection: Shared Pathways and Mechanisms
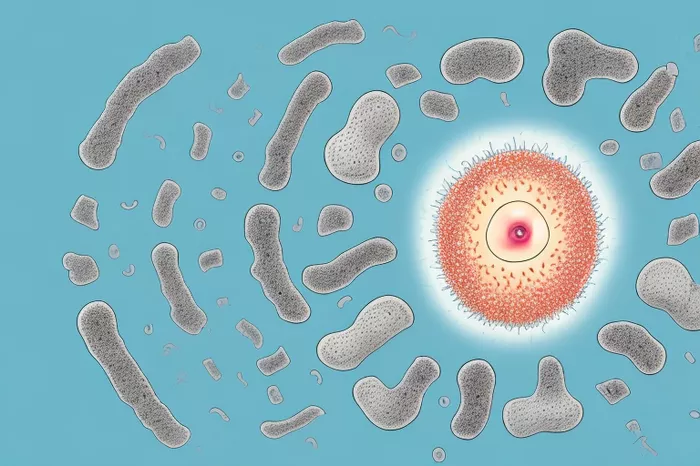
Immunological dysregulation lies at the heart of both eczema and asthma. In eczema, the skin’s immune response is heightened, leading to inflammation and skin barrier dysfunction. This inflammatory milieu can trigger systemic immune responses and predispose individuals to allergic sensitization, not only in the skin but also in the respiratory tract.
In asthma, the airway inflammation is characterized by increased levels of pro-inflammatory cytokines, infiltration of immune cells, and airway hyperresponsiveness. Interestingly, similar inflammatory pathways involving T-helper type 2 (Th2) cells, eosinophils, and mast cells are implicated in both eczema and asthma, indicating a shared immunological basis.
The Hygiene Hypothesis: Environmental Factors and Their Influence
The hygiene hypothesis proposes that reduced exposure to infections and microbial agents in early childhood may lead to an increased risk of allergic diseases. While the hypothesis primarily relates to asthma, it also has implications for eczema.
Children growing up in overly clean and sanitized environments may have a less diverse microbial exposure, affecting the development and maturation of their immune systems. This altered immune response may predispose individuals to allergic sensitization and the subsequent development of eczema and asthma.
The Role of Allergic Sensitization: IgE-Mediated Responses
Allergic sensitization, characterized by the production of immunoglobulin E (IgE) antibodies in response to allergens, is a hallmark feature of both eczema and asthma. Individuals with eczema often have elevated levels of serum IgE and are more prone to developing allergic rhinitis and asthma later in life.
The presence of allergic sensitization suggests a common underlying mechanism driving both conditions. Exposure to common allergens, such as house dust mites, pollen, and pet dander, can trigger allergic reactions in both the skin and the airways, contributing to the development and exacerbation of eczema and asthma.
The Impact of Environmental Triggers: Allergens, Irritants, and Air Pollution
Environmental factors play a significant role in triggering and exacerbating both eczema and asthma. Allergens such as pollen, mold, dust mites, and pet dander can induce allergic reactions in susceptible individuals, leading to flare-ups of eczema and asthma symptoms.
Moreover, exposure to irritants such as tobacco smoke, air pollution, and harsh chemicals can exacerbate inflammation and worsen symptoms in both conditions. The effect of environmental triggers underscores the importance of environmental control measures and lifestyle modifications in managing eczema and asthma.
The Bidirectional Relationship: Understanding the Impact of Eczema on Asthma and Vice Versa
The relationship between eczema and asthma is bidirectional, with each condition influencing the other’s course and severity. Individuals with severe eczema are at an increased risk of developing asthma, particularly if the eczema begins in early childhood.
Conversely, asthma exacerbations can trigger eczema flares through systemic inflammation and immune dysregulation. The presence of eczema in children with asthma is associated with more severe asthma symptoms and poorer asthma control, highlighting the interplay between these two conditions.
Implications for Management and Treatment: A Holistic Approach
Given the complex interconnection between eczema and asthma, a holistic approach to management is essential. Treatment strategies should aim to address both conditions simultaneously, focusing on controlling inflammation, managing symptoms, and minimizing triggers.
Topical corticosteroids and emollients are mainstays of eczema management, while inhaled corticosteroids and bronchodilators are commonly used to control asthma symptoms. Allergen avoidance, proper skin care, and environmental control measures are vital components of comprehensive management plans for individuals with both eczema and asthma.
Conclusion
In summary, eczema and asthma are closely related conditions with shared genetic, immunological, and environmental factors contributing to their development and progression. Understanding the intricate interplay between these conditions is crucial for providing optimal care and improving outcomes for affected individuals.
By recognizing and addressing the underlying mechanisms driving eczema and asthma, healthcare professionals can tailor treatment approaches to target both conditions effectively. Moreover, ongoing research aimed at elucidating the complex relationship between eczema and asthma holds promise for the development of novel therapeutic strategies and interventions.
Ultimately, a multifaceted approach that considers the interconnected nature of eczema and asthma is essential for providing comprehensive care and improving the quality of life for individuals affected by these chronic inflammatory conditions.
Related Topics:
What Is the Fastest Way to Cure Dyshidrotic Eczema