Psoriasis, a chronic autoimmune condition, manifests in various forms and severities, impacting millions worldwide. Among its diverse presentations, acute psoriasis stands out for its sudden onset and often intense symptoms. Understanding these symptoms is crucial for timely diagnosis, effective management, and improved quality of life for those affected. In this comprehensive guide, we delve into the distinctive signs and symptoms of acute psoriasis, shedding light on its clinical manifestations and their implications for patients and healthcare providers alike.
What is Psoriasis?
Before delving into the specifics of acute psoriasis symptoms, it’s essential to grasp the fundamentals of the condition itself. Psoriasis is a chronic autoimmune disorder characterized by rapid skin cell proliferation, leading to the formation of thick, scaly plaques. While its exact cause remains elusive, genetic predisposition, immune system dysfunction, and environmental factors are believed to contribute to its development.
Understanding Acute Psoriasis: An Overview
Acute psoriasis represents a flare-up or exacerbation of the condition, often marked by sudden onset and intense symptoms. While individuals with chronic psoriasis may experience periods of remission, acute episodes can arise unexpectedly, significantly impacting their physical and emotional well-being.
Symptoms of Acute Psoriasis
1. Rapidly Spreading Plaques: One of the hallmark symptoms of acute psoriasis is the sudden appearance of inflamed, raised patches of skin, known as plaques. These plaques are typically red or pink in color and covered with silvery scales, imparting a distinct appearance.
2. Severe Itching and Discomfort: Acute psoriasis is often accompanied by intense itching, which can interfere with daily activities and disrupt sleep patterns. The constant urge to scratch affected areas can exacerbate inflammation and lead to secondary infections.
3. Pain and Tenderness: In addition to itching, individuals experiencing acute psoriasis may report pain and tenderness in affected areas. This discomfort can vary in intensity and may be exacerbated by friction or pressure on the skin.
4. Joint Involvement (Psoriatic Arthritis): In some cases, acute psoriasis may coincide with the onset of psoriatic arthritis, a condition characterized by joint inflammation and stiffness. Commonly affected joints include those of the hands, feet, knees, and spine, leading to reduced mobility and functional impairment.
5. Nail Changes: Psoriasis can also affect the nails, causing various abnormalities such as pitting, discoloration, thickening, and separation from the nail bed. These changes can be particularly distressing for individuals, impacting both aesthetics and function.
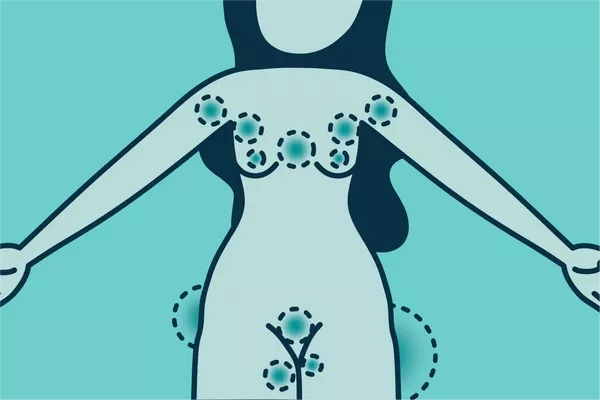
6. Inverse Psoriasis: While classic psoriasis plaques typically appear on extensor surfaces such as the elbows and knees, acute psoriasis may manifest in less typical locations, including skin folds such as the groin, armpits, and beneath the breasts. This variant, known as inverse psoriasis, presents as smooth, red patches that worsen with friction and sweating.
7. Guttate Psoriasis: Another form of acute psoriasis, known as guttate psoriasis, is characterized by small, red spots that resemble drops or tear-shaped lesions. This subtype often develops following a bacterial or viral infection and may affect large areas of the body, including the trunk, limbs, and scalp.
Diagnosis and Differential Diagnosis
Diagnosing acute psoriasis typically involves a thorough clinical evaluation, including a review of symptoms, medical history, and physical examination. Dermatologists may also perform a skin biopsy to confirm the diagnosis and rule out other skin conditions with similar presentations. Differential diagnosis may include eczema, seborrheic dermatitis, fungal infections, and allergic reactions, among others.
Treatment and Management Strategies
Effective management of acute psoriasis requires a multidisciplinary approach tailored to the individual needs of each patient. While there is no cure for psoriasis, various treatment modalities can help alleviate symptoms, reduce inflammation, and promote skin healing. Treatment options may include:
1. Topical Therapies: Corticosteroids, vitamin D analogs, retinoids, and calcineurin inhibitors are commonly prescribed topical agents for the treatment of psoriasis plaques. These medications help reduce inflammation, suppress excessive cell turnover, and alleviate symptoms such as itching and scaling.
2. Phototherapy: Phototherapy, or light therapy, involves exposing the skin to controlled doses of ultraviolet (UV) radiation to reduce inflammation and slow down cell proliferation. Both narrowband UVB and psoralen plus ultraviolet A (PUVA) therapy have been shown to be effective in the management of psoriasis.
3. Systemic Medications: For severe or refractory cases of acute psoriasis, systemic medications such as oral retinoids, methotrexate, cyclosporine, and biologic agents may be prescribed. These medications target the underlying immune dysfunction responsible for psoriasis flare-ups, helping to control symptoms and prevent disease progression.
4. Lifestyle Modifications: Adopting a healthy lifestyle can complement medical treatment and help manage psoriasis symptoms more effectively. Strategies such as stress reduction, maintaining a balanced diet, avoiding triggers such as smoking and excessive alcohol consumption, and practicing good skincare can contribute to overall well-being and symptom relief.
5. Patient Education and Support: Empowering patients with knowledge about their condition and self-care strategies is essential for long-term management success. Healthcare providers play a vital role in educating patients about psoriasis, discussing treatment options, addressing concerns, and providing ongoing support and encouragement.
Conclusion
Acute psoriasis poses significant challenges for individuals affected by this chronic autoimmune condition, impacting both physical comfort and emotional well-being. Recognizing the distinctive signs and symptoms of acute psoriasis is crucial for timely diagnosis and effective management, enabling patients to regain control of their lives and minimize the impact of flare-ups on their daily activities. By understanding the underlying mechanisms of psoriasis and implementing personalized treatment approaches, healthcare providers can help improve outcomes and enhance the quality of life for individuals living with this complex dermatological condition.
Related Topics: