Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory skin condition that affects the apocrine sweat glands, leading to the formation of painful nodules, abscesses, and scarring. This debilitating disease significantly impacts the quality of life of those affected and is often associated with various comorbidities. Understanding the diseases associated with HS is crucial for comprehensive patient care and effective management strategies.
The Pathophysiology of Hidradenitis Suppurativa
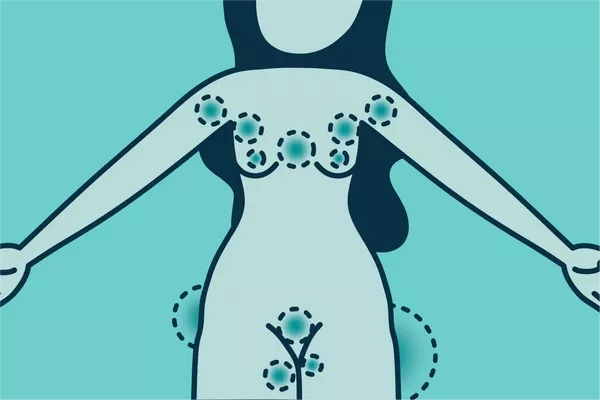
HS typically manifests after puberty and is characterized by recurrent and painful skin lesions in areas with a high density of apocrine glands, such as the armpits, groin, buttocks, and under the breasts. The exact cause of HS remains unclear, but it is believed to involve a combination of genetic, hormonal, and environmental factors. The inflammation in HS is thought to begin in the hair follicles, leading to the formation of painful nodules and sinus tracts that can become secondarily infected.
Metabolic Syndrome and Cardiovascular Disease
1. Metabolic Syndrome
One of the most significant associations with HS is metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. These conditions include increased blood pressure, high blood sugar levels, excess body fat around the waist, and abnormal cholesterol levels. Studies have shown that patients with HS are at a higher risk of developing metabolic syndrome compared to the general population. The chronic inflammation seen in HS is believed to contribute to insulin resistance and dyslipidemia, key components of metabolic syndrome.
2. Cardiovascular Disease
Closely linked to metabolic syndrome is cardiovascular disease. HS patients are at an increased risk for atherosclerosis, which can lead to coronary artery disease, myocardial infarction, and stroke. The chronic inflammatory state in HS contributes to endothelial dysfunction and arterial stiffness, both of which are precursors to cardiovascular disease. It is crucial for clinicians to monitor cardiovascular health in HS patients and manage risk factors aggressively.
3. Diabetes Mellitus
Diabetes mellitus, particularly type 2 diabetes, has a well-documented association with HS. The prevalence of diabetes is higher in individuals with HS than in the general population. Chronic inflammation and insulin resistance, common in both conditions, may explain this relationship. Additionally, the physical and psychological stress associated with managing a chronic condition like HS can further exacerbate blood glucose control, making diabetes management more challenging in these patients.
Inflammatory Bowel Disease
1. Crohn’s Disease
Inflammatory bowel disease (IBD), particularly Crohn’s disease, is another condition frequently associated with HS. Both diseases share similar immunopathological features, such as dysregulation of the immune system and chronic inflammation. Crohn’s disease can affect any part of the gastrointestinal tract, leading to symptoms like abdominal pain, diarrhea, and weight loss. The coexistence of HS and Crohn’s disease suggests a shared genetic and inflammatory pathway. Patients with both conditions may experience more severe disease courses, requiring multidisciplinary management.
2. Ulcerative Colitis
Although less common than Crohn’s disease, ulcerative colitis (UC) is also associated with HS. UC affects the colon and rectum, leading to chronic inflammation and ulceration of the colon’s lining. The link between HS and UC is not as strong as with Crohn’s disease, but it underscores the systemic inflammatory nature of HS and the need for comprehensive evaluation of patients presenting with HS and gastrointestinal symptoms.
Spondyloarthropathies
1. Ankylosing Spondylitis
HS is associated with a higher prevalence of spondyloarthropathies, a group of inflammatory rheumatic diseases that includes ankylosing spondylitis (AS). AS primarily affects the spine and sacroiliac joints, leading to chronic pain and progressive spinal stiffness. The exact link between HS and AS is not fully understood, but both conditions involve chronic inflammation and a potential genetic predisposition involving the HLA-B27 gene. Patients with HS should be evaluated for symptoms of AS, such as chronic back pain and stiffness, particularly if they exhibit features of spondyloarthropathy.
2. Psoriatic Arthritis
Psoriatic arthritis (PsA) is another spondyloarthropathy associated with HS. PsA is characterized by joint inflammation and skin lesions similar to psoriasis. The association between HS and PsA suggests a shared pathophysiological mechanism, potentially involving dysregulation of the immune system. Patients with HS and PsA may experience severe joint symptoms, requiring a combination of dermatologic and rheumatologic care for optimal management.
Dermatological Comorbidities
1. Acne and Pilonidal Cysts
Patients with HS often present with other dermatological conditions such as severe acne and pilonidal cysts. Severe acne, like HS, involves inflammation of the hair follicles and can lead to the formation of painful nodules and scarring. Pilonidal cysts occur in the crease of the buttocks and can become infected, forming painful abscesses. The co-occurrence of these conditions may reflect a shared susceptibility to follicular occlusion and inflammation.
2. Psoriasis
Psoriasis is a chronic inflammatory skin disease characterized by red, scaly patches. It shares common immunological pathways with HS, involving cytokines such as TNF-alpha and IL-17. The co-occurrence of psoriasis and HS can complicate the clinical picture, requiring integrated treatment approaches to manage both skin conditions effectively.
Psychological Disorders
1. Depression and Anxiety
The chronic pain, disfigurement, and social stigma associated with HS can lead to significant psychological distress. Depression and anxiety are common among HS patients, often exacerbated by the chronic nature of the disease and the impact on quality of life. Addressing mental health is a critical component of comprehensive HS management, requiring collaboration between dermatologists and mental health professionals.
2. Body Dysmorphic Disorder
Body dysmorphic disorder (BDD) is characterized by an obsessive focus on perceived flaws in appearance, which can be particularly relevant in HS due to the visible skin lesions and scarring. Patients with HS and BDD may engage in excessive skin picking or avoidance of social interactions, further impacting their mental health and quality of life. Treatment for BDD often involves cognitive-behavioral therapy and, in some cases, medication.
Autoimmune Disorders
1. Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that can affect multiple organ systems, including the skin, joints, kidneys, and nervous system. There is evidence to suggest an association between HS and SLE, likely due to shared autoimmune mechanisms. Patients with HS who exhibit systemic symptoms such as joint pain, fatigue, and photosensitivity should be evaluated for SLE to ensure prompt and appropriate management.
2. Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune condition that primarily affects the joints, leading to pain, swelling, and potential joint deformity. While the direct association between HS and RA is less clear, the presence of chronic inflammation in both conditions suggests a possible link. Screening for RA in patients with HS may be warranted if they present with persistent joint symptoms.
Hormonal Disorders
1. Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) is a common hormonal disorder among women of reproductive age, characterized by irregular menstrual periods, excess androgen levels, and polycystic ovaries. There is a notable association between HS and PCOS, potentially due to the role of androgens in the pathogenesis of both conditions. Women with HS should be evaluated for symptoms of PCOS, such as menstrual irregularities and hirsutism, as part of a holistic approach to their care.
Infectious Diseases
1. Human Immunodeficiency Virus (HIV)
Patients with HS have a higher prevalence of HIV infection compared to the general population. The immunosuppressive nature of HIV may exacerbate the inflammatory process in HS, leading to more severe and recurrent skin lesions. Early diagnosis and treatment of HIV in HS patients are crucial to managing both conditions effectively and improving overall prognosis.
2. Chronic Infections
Chronic bacterial and fungal infections can complicate the course of HS, particularly in areas of recurrent abscess formation. Patients with HS may require long-term antibiotic therapy or surgical interventions to manage these infections, highlighting the need for vigilant monitoring and prompt treatment of infectious complications.
Conclusion
Hidradenitis suppurativa is a multifaceted disease with a broad spectrum of associated comorbidities. Understanding these associations is essential for providing comprehensive care to patients with HS. The links between HS and metabolic syndrome, cardiovascular disease, diabetes mellitus, inflammatory bowel disease, spondyloarthropathies, dermatological conditions, psychological disorders, autoimmune diseases, hormonal disorders, and infectious diseases underscore the systemic nature of HS and the need for a multidisciplinary approach to treatment. Clinicians must be vigilant in screening for these comorbidities and implementing integrated management strategies to improve patient outcomes and quality of life. Through ongoing research and collaboration, the medical community can continue to enhance our understanding and management of hidradenitis suppurativa and its associated diseases.
Related Topics: