Hidradenitis Suppurativa (HS) is a chronic skin condition characterized by painful, recurrent nodules, abscesses, and tunnels that typically develop in areas where skin rubs together, such as the armpits, groin, buttocks, and under the breasts. This condition can significantly impact a person’s quality of life, both physically and emotionally. Managing HS requires a multidisciplinary approach that addresses the symptoms, underlying causes, and the psychosocial aspects of the condition. In this article, we will explore the various treatment options available, ranging from medical interventions to lifestyle modifications.
Understanding Hidradenitis Suppurativa:
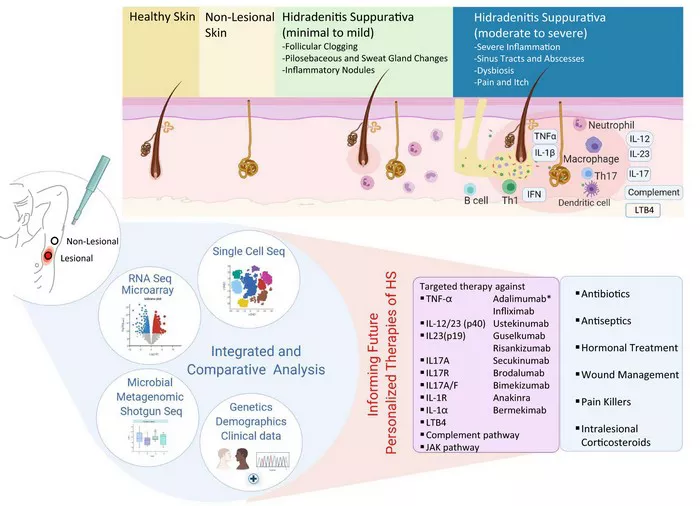
Before delving into treatment strategies, it is essential to understand the underlying factors contributing to Hidradenitis Suppurativa. While the exact cause remains unclear, several factors, including genetics, inflammation, and lifestyle, may play a role in its development. The condition often begins after puberty and is more common in individuals with a family history of HS. Obesity and metabolic syndrome have also been identified as potential risk factors.
Medical Treatments:
1. Topical and Oral Antibiotics:
Antibiotics, both topical and oral, are commonly prescribed to manage HS. These medications help control bacterial infections that often accompany the condition. Topical antibiotics may be applied directly to affected areas, while oral antibiotics like tetracycline or clindamycin can be prescribed for more widespread involvement.
2. Corticosteroids:
Corticosteroids can help reduce inflammation and alleviate pain associated with HS. However, long-term use of corticosteroids may have side effects, so their use is often limited to short periods or for acute flare-ups.
3. Biologics:
Biologic medications, such as adalimumab, have shown promise in treating moderate to severe cases of Hidradenitis Suppurativa. These drugs target specific components of the immune system to reduce inflammation and prevent flare-ups.
4. Hormonal Therapies:
For women with HS, hormonal therapies like oral contraceptives or anti-androgen medications may be considered. These treatments aim to regulate hormones that can contribute to the development of the condition.
Surgical Interventions:
1. Incision and Drainage:
In cases where abscesses have formed, incision and drainage may be necessary. This procedure involves making a small incision to release accumulated pus and alleviate pain.
2. Laser and Light Therapies:
Laser and light therapies, such as carbon dioxide laser or intense pulsed light (IPL), can help reduce inflammation and improve the appearance of scars. These treatments target the hair follicles and sebaceous glands, which are often implicated in HS.
3. Excisional Surgery:
In severe cases, where nodules and tunnels are extensive, excisional surgery may be recommended. This involves removing affected skin and underlying tissue to promote healing. While this approach can provide long-term relief, it is reserved for cases that do not respond to other treatments.
Lifestyle Modifications:
1. Weight Management:
Given the association between obesity and Hidradenitis Suppurativa, weight management plays a crucial role in treatment. Adopting a healthy diet and engaging in regular physical activity can help reduce inflammation and improve overall well-being.
2. Personal Hygiene:
Maintaining good personal hygiene is essential in managing HS. Regular cleansing of affected areas and using antibacterial soaps can help prevent bacterial overgrowth and reduce the risk of infections.
3. Avoiding Tight Clothing:
Wearing loose-fitting clothing can minimize friction and irritation, reducing the likelihood of new flare-ups. Avoiding tight clothing in areas prone to HS lesions is particularly important.
Psychosocial Support:
1. Counseling and Support Groups:
Living with Hidradenitis Suppurativa can take a toll on one’s mental health. Counseling and participation in support groups can provide emotional support, coping strategies, and a sense of community for individuals dealing with this challenging condition.
2. Educational Resources:
Providing patients with educational resources about Hidradenitis Suppurativa can empower them to better understand their condition and actively participate in their treatment plans. This includes information about triggers, symptom management, and the importance of early intervention.
Conclusion
Effectively managing Hidradenitis Suppurativa requires a comprehensive approach that addresses the medical, surgical, lifestyle, and psychosocial aspects of the condition. Tailoring treatment plans to individual needs, involving patients in decision-making, and staying informed about emerging therapies are crucial steps in enhancing outcomes for those affected by HS. By combining medical interventions with lifestyle modifications and psychosocial support, healthcare professionals can work collaboratively with patients to minimize the impact of Hidradenitis Suppurativa on their lives.