Ringworm, despite its name, is not caused by a worm but rather by a fungal infection. This common skin condition, medically known as dermatophytosis, can affect people of all ages and backgrounds. One of the key aspects in managing ringworm effectively is recognizing its symptoms early on. However, the timing of symptom onset can vary depending on several factors. In this article, we delve into the nuances of ringworm, exploring when symptoms typically appear and the factors that influence their onset.
What is Ringworm?
Before diving into the timing of symptoms, it’s crucial to understand what ringworm is and how it spreads. Ringworm is a contagious fungal infection that can affect the skin, scalp, and nails. Despite its name, it’s not caused by a worm but by various fungi known as dermatophytes, which thrive in warm, moist environments.
These fungi can be found in soil, on surfaces, and even on the skin of humans and animals. Ringworm is highly contagious and can spread through direct skin-to-skin contact with an infected person or animal, or by touching contaminated objects or surfaces.
The Stages of Ringworm Infection
Ringworm infection typically progresses through several stages, each characterized by distinct symptoms. Understanding these stages can provide insight into when symptoms might appear.
1. Incubation Period:
After coming into contact with the fungus, there is a period of incubation before symptoms develop. During this time, the fungus begins to grow and multiply on the skin or other affected areas. The length of the incubation period can vary depending on factors such as the type of fungus and the individual’s immune response.
2. Initial Symptoms:
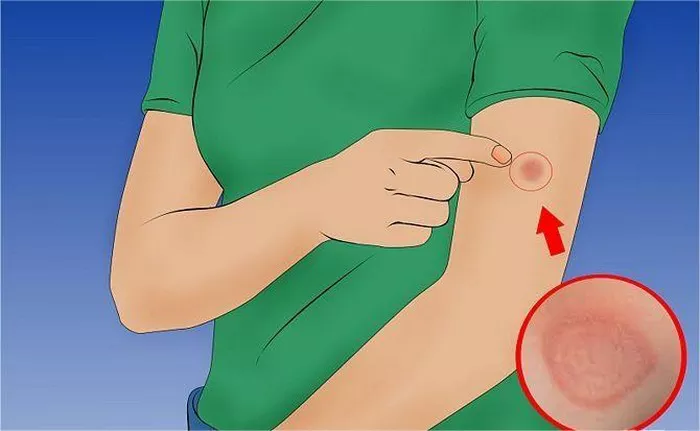
The first signs of ringworm often appear within 4 to 14 days after exposure to the fungus. However, it’s essential to note that this timeframe can vary widely. Initial symptoms may include redness, itching, and the formation of small, raised bumps or patches on the skin. These patches may have defined borders and a slightly raised, scaly texture.
3. Progression of Symptoms:
Without treatment, ringworm can progress, leading to the enlargement of the affected area and the development of additional patches. The itching and discomfort associated with the infection may also intensify as it spreads. In some cases, the affected skin may become inflamed and blistered, particularly in areas where friction occurs, such as between the toes or in the groin area.
4. Chronic or Recurrent Infection:
In some instances, ringworm may become chronic or recurrent, persisting for weeks or even months. Factors such as compromised immune function, underlying health conditions, and inadequate treatment can contribute to the persistence of the infection.
Factors Influencing Symptom Onset
Several factors can influence when symptoms of ringworm appear and how they manifest. These factors can vary from individual to individual and may include:
1. Type of Fungus:
Different species of dermatophytes can cause ringworm, and the timing and severity of symptoms may vary depending on the specific fungus involved. Some species may produce more aggressive infections, leading to faster onset of symptoms and more severe manifestations.
2. Site of Infection:
The location of the ringworm infection on the body can also impact symptom onset. For example, ringworm on areas of the body with thinner skin, such as the face or neck, may become symptomatic more quickly than infections on thicker-skinned areas like the arms or legs.
3. Individual Immune Response:
The immune response of the individual plays a significant role in determining how quickly symptoms appear and how effectively the body can combat the infection. Individuals with weakened immune systems, such as those with certain medical conditions or undergoing immunosuppressive therapy, may experience delayed symptom onset or more severe infections.
4. Environmental Factors:
Environmental factors, such as humidity and temperature, can create ideal conditions for fungal growth and proliferation. Warmer, more humid environments provide optimal conditions for dermatophytes to thrive, potentially accelerating symptom onset and exacerbating the infection.
5. Personal Hygiene Practices:
Good personal hygiene practices, including regular handwashing and keeping the skin clean and dry, can help reduce the risk of ringworm infection and minimize the severity of symptoms. Conversely, poor hygiene practices can increase the likelihood of infection and contribute to more prolonged or recurrent cases.
Recognizing and Managing Ringworm Symptoms
Early recognition of ringworm symptoms is essential for prompt treatment and effective management of the infection. If you suspect you or someone you know may have ringworm, it’s crucial to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Common treatment options for ringworm may include topical antifungal medications, oral antifungal agents, and medicated shampoos for scalp infections. In addition to medication, practicing good hygiene, avoiding sharing personal items such as clothing and towels, and disinfecting surfaces can help prevent the spread of ringworm to others and reduce the risk of recurrent infections.
Conclusion
In conclusion, the timing of ringworm symptoms can vary depending on a variety of factors, including the type of fungus, the site of infection, individual immune response, environmental conditions, and personal hygiene practices. By understanding these factors and recognizing the early signs of infection, individuals can take proactive steps to seek treatment and minimize the impact of ringworm on their health and well-being.