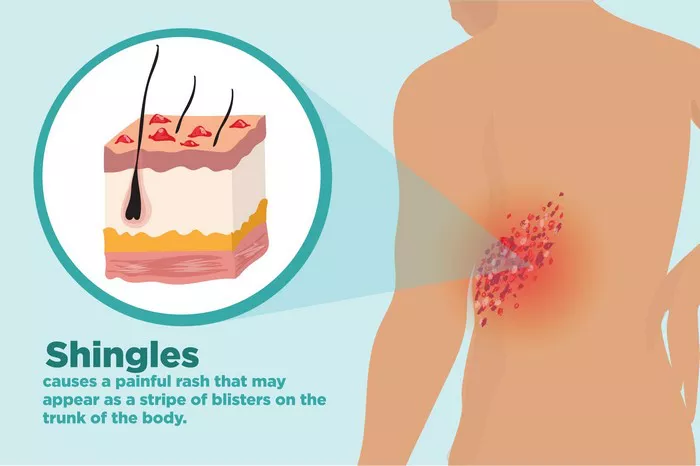
Shingles, medically known as herpes zoster, is a viral infection caused by the varicella-zoster virus—the same virus that causes chickenpox. It typically manifests as a painful rash with blisters on one side of the body, often in a band-like pattern. While shingles is a distinctive condition with its characteristic symptoms, there are other diseases that share similarities, either in their presentation or underlying mechanisms. Understanding these diseases and their nuances is crucial for accurate diagnosis and effective management. In this article, we delve into the realm of diseases akin to shingles, shedding light on their features, diagnostic considerations, and treatment approaches.
Similarities in Symptomatology
One of the primary diseases that bears resemblance to shingles is herpes simplex virus (HSV) infection, particularly herpes simplex dermatitis. HSV is a DNA virus belonging to the Herpesviridae family, just like the varicella-zoster virus. While herpes simplex dermatitis typically presents with grouped vesicles or blisters on an erythematous base, similar to shingles, it commonly affects the face or genitals rather than following a dermatomal distribution. However, in rare instances, herpes simplex dermatitis can mimic shingles, especially when it affects the trunk or extremities.
Another condition often confused with shingles is herpes zoster oticus, also known as Ramsay Hunt syndrome. This disorder results from the reactivation of the varicella-zoster virus in the geniculate ganglion of the facial nerve. Unlike typical shingles, herpes zoster oticus manifests with vesicles in the ear canal, ear pain, facial paralysis, and sometimes vertigo. While the involvement of the facial nerve distinguishes it from classical shingles, the similarity in viral etiology and dermatomal distribution can lead to diagnostic challenges.
Furthermore, dermatological conditions such as contact dermatitis, allergic reactions, and insect bites can mimic shingles, primarily due to their shared feature of vesicular eruptions. These conditions often necessitate careful examination and, at times, diagnostic tests to differentiate them from shingles accurately.
Underlying Mechanisms and Etiology
To comprehend diseases akin to shingles comprehensively, it is imperative to delve into their underlying mechanisms and etiology. Shingles and its counterparts often stem from viral infections, with varicella-zoster virus and herpes simplex virus being the primary culprits. These viruses belong to the herpesvirus family, characterized by their ability to establish latent infections in nerve cells, paving the way for reactivation and subsequent disease manifestation.
The reactivation of latent viruses is a central theme in the pathogenesis of shingles and related conditions. Factors such as aging, immunosuppression, and stress can weaken the immune response, allowing the dormant virus to reactivate and cause disease. This phenomenon underscores the importance of immunocompetence in controlling viral infections and preventing their recurrence.
Moreover, the dermatomal distribution of lesions in shingles and similar conditions is attributed to the anatomical arrangement of sensory nerves. Following primary infection or vaccination with varicella-zoster virus, the virus establishes latency in the dorsal root ganglia. Upon reactivation, it travels along sensory nerve fibers, leading to inflammation and the characteristic rash in the corresponding dermatome. Similarly, herpes simplex virus can also follow sensory nerve pathways, albeit with different dermatomal involvement.
Diagnostic Considerations
Accurate diagnosis forms the cornerstone of effective management for diseases resembling shingles. While clinical evaluation plays a pivotal role, laboratory tests and diagnostic procedures may be necessary to confirm the diagnosis and rule out differential diagnoses.
In the case of suspected shingles, the presence of a painful, unilateral rash with grouped vesicles or blisters following a dermatomal distribution is highly suggestive. However, in atypical presentations or when clinical uncertainty exists, laboratory tests such as viral culture, polymerase chain reaction (PCR), or direct fluorescent antibody (DFA) testing can aid in confirming the diagnosis.
Distinguishing shingles from herpes simplex dermatitis or herpes zoster oticus may require additional evaluation, including otoscopy for herpes zoster oticus and serological testing for herpes simplex virus. Moreover, considering the possibility of dermatological mimickers, a comprehensive history, including recent exposures and medication use, coupled with skin biopsy or patch testing, may be warranted.
Treatment Approaches
Management strategies for diseases akin to shingles encompass antiviral therapy, pain management, and supportive care. Antiviral medications such as acyclovir, valacyclovir, and famciclovir are the mainstay of treatment for shingles and herpes simplex infections. Early initiation of antiviral therapy within 72 hours of rash onset can hasten lesion healing, alleviate pain, and reduce the risk of complications.
In addition to antiviral therapy, pain management plays a crucial role in improving patient outcomes, especially in conditions associated with significant discomfort such as shingles. Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and topical agents such as lidocaine or capsaicin cream can provide symptomatic relief. In cases of neuropathic pain or persistent discomfort, adjuvant therapies including tricyclic antidepressants, anticonvulsants, or opioids may be considered under close monitoring.
Furthermore, supportive measures such as rest, hydration, and proper wound care are vital components of holistic management for patients with shingles or related conditions. Educating patients about the importance of medication adherence, symptom monitoring, and preventive measures to reduce transmission is paramount in preventing disease recurrence and minimizing complications.
Conclusion
In conclusion, while shingles is a distinctive condition with its characteristic rash and symptoms, several diseases share similarities either in their clinical presentation or underlying mechanisms. Herpes simplex dermatitis, herpes zoster oticus, and dermatological mimickers pose diagnostic challenges and necessitate a comprehensive approach to evaluation and management. Understanding the nuances of these diseases, including their symptomatology, pathogenesis, and treatment approaches, is essential for healthcare providers to deliver optimal care and improve patient outcomes. By unraveling the mystery surrounding diseases akin to shingles, we can enhance diagnostic accuracy, streamline therapeutic interventions, and ultimately alleviate the burden of these conditions on affected individuals.