Hidradenitis Suppurativa (HS) is a chronic inflammatory skin condition characterized by painful, recurrent nodules, abscesses, and sinus tracts primarily affecting the intertriginous areas of the body, such as the axillae, groin, and buttocks. While HS can significantly impact a person’s quality of life due to pain, discomfort, and psychological distress, the question of whether it can be fatal often arises among those diagnosed with this condition.
To address this concern, it’s crucial to understand the nature of HS, its potential complications, and how it can impact overall health and well-being.
Understanding Hidradenitis Suppurativa
HS is a complex disorder that involves the inflammation of hair follicles and apocrine glands, leading to the formation of painful nodules, abscesses, and tunnels beneath the skin’s surface. The exact cause of HS remains unclear, but it is believed to involve a combination of genetic predisposition, immune dysfunction, and environmental factors.
The disease typically manifests during or after puberty and tends to worsen over time, with recurrent flare-ups and periods of remission. The severity of HS varies among individuals, ranging from mild, where symptoms are relatively manageable, to severe, where large areas of skin are affected, leading to significant pain, scarring, and limited mobility.
Potential Complications of Hidradenitis Suppurativa
While HS primarily affects the skin, it can have far-reaching consequences beyond dermatological symptoms. Some of the potential complications associated with HS include:
1. Secondary Infections: The open wounds and sinus tracts characteristic of HS create an environment conducive to bacterial growth, increasing the risk of secondary infections. These infections can be localized or systemic, potentially leading to cellulitis, abscess formation, or even sepsis if left untreated.
2. Scarring and Disfigurement: Chronic inflammation and recurrent flare-ups can result in extensive scarring and tissue damage, leading to disfigurement of affected areas. Severe scarring can impair mobility and cause psychological distress, impacting an individual’s overall quality of life.
3. Reduced Quality of Life: The chronic pain, discomfort, and embarrassment associated with HS can significantly diminish a person’s quality of life, affecting their ability to work, engage in social activities, and maintain relationships. Depression, anxiety, and social isolation are common among individuals living with severe HS.
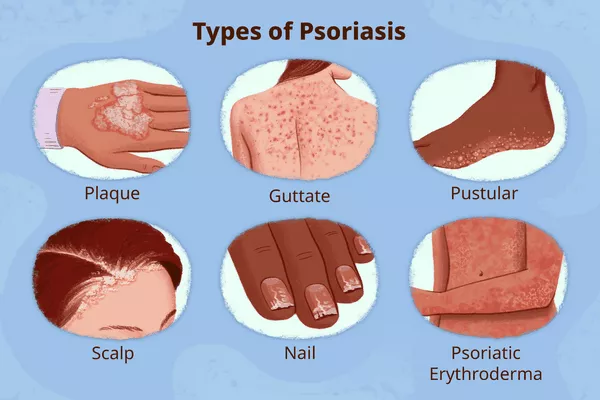
4. Associated Conditions: Studies have shown that individuals with HS have a higher prevalence of certain comorbidities, including obesity, metabolic syndrome, inflammatory bowel disease, and depression. These conditions can further exacerbate the impact of HS on overall health and well-being.
Mortality Risk and Hidradenitis Suppurativa
While HS itself is not directly life-threatening, the condition can contribute to an increased risk of mortality through its associated complications and comorbidities. For example:
1. Sepsis: Severe cases of HS with widespread infection can lead to sepsis, a potentially life-threatening condition characterized by systemic inflammation and organ dysfunction. Prompt medical intervention is crucial to prevent sepsis from becoming fatal.
2. Cardiovascular Disease: Some studies have suggested an association between HS and an increased risk of cardiovascular disease, including heart attacks and strokes. Chronic inflammation, which is a hallmark of HS, may contribute to the development and progression of cardiovascular conditions over time.
3. Suicidal Behavior: The chronic pain, disfigurement, and psychological impact of HS can take a significant toll on mental health, increasing the risk of depression, anxiety, and suicidal behavior. It’s essential for individuals with HS to receive adequate support and mental health care to address these concerns.
Treatment and Management Strategies
While there is currently no cure for HS, various treatment options are available to manage symptoms, reduce inflammation, and prevent complications. Treatment approaches may include:
1. Topical and Oral Medications: Antibiotics, anti-inflammatory drugs, and immunosuppressants may be prescribed to control infection, reduce inflammation, and alleviate pain associated with HS flare-ups.
2. Lifestyle Modifications: Maintaining good hygiene practices, wearing loose-fitting clothing, and avoiding activities that may exacerbate friction or sweating can help reduce the frequency and severity of HS flare-ups.
3. Surgical Interventions: In severe cases of HS that do not respond to conservative treatments, surgical procedures such as incision and drainage of abscesses, excision of affected tissue, or laser therapy may be recommended to improve symptoms and prevent recurrence.
4. Biologic Therapies: Emerging biologic medications, such as tumor necrosis factor-alpha (TNF-alpha) inhibitors and interleukin inhibitors, have shown promise in the treatment of HS by targeting specific pathways involved in the inflammatory process.
Conclusion
While Hidradenitis Suppurativa is not directly fatal, it can have significant implications for an individual’s overall health and well-being due to its associated complications and comorbidities. The chronic nature of the disease, coupled with its impact on physical and mental health, underscores the importance of early diagnosis, comprehensive management, and multidisciplinary care.
By addressing symptoms, preventing complications, and addressing underlying risk factors, individuals with HS can improve their quality of life and reduce the long-term impact of the disease on their health. Moreover, raising awareness about HS among healthcare professionals, policymakers, and the general public is crucial for promoting timely intervention and improving outcomes for those affected by this often misunderstood condition.