Eczema, a chronic inflammatory skin condition, affects millions worldwide, presenting in various forms and locations on the body. Among its manifestations, eczema on the scalp poses unique challenges and discomfort for those afflicted. Understanding the intricacies of what causes eczema on the head is pivotal in devising effective management strategies for individuals grappling with this condition.
Introduction to Eczema on the Scalp
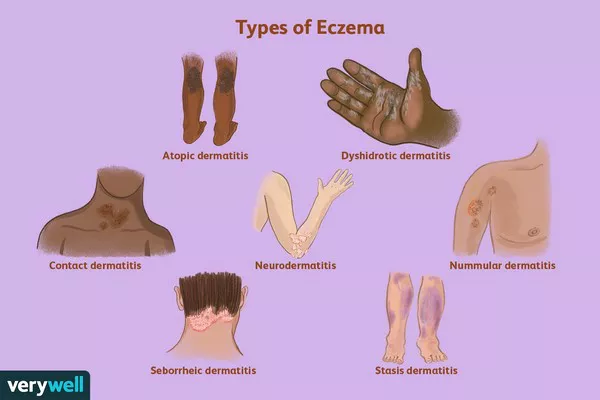
Eczema, also known as atopic dermatitis, is characterized by dry, itchy, inflamed skin patches. While its exact cause remains elusive, eczema is believed to result from a combination of genetic, environmental, and immunological factors. Its appearance on the scalp can be particularly bothersome, as the itching and flaking associated with scalp eczema can impact daily activities and quality of life.
The Role of Genetics
Genetic predisposition plays a significant role in the development of eczema. Individuals with a family history of eczema, asthma, or allergic rhinitis are more likely to develop the condition themselves. Several genes associated with skin barrier function and immune response have been implicated in eczema susceptibility. Variations in these genes can compromise the skin’s ability to retain moisture and protect against environmental irritants, making individuals more prone to developing eczema, including on the scalp.
Immune Dysfunction and Inflammation
The immune system’s response to environmental triggers is central to the development of eczema. In individuals with eczema, the immune system overreacts to certain substances, such as allergens or irritants, leading to inflammation and skin damage. This immune dysfunction can manifest on the scalp, where exposure to hair care products, sweat, and environmental pollutants may exacerbate inflammation and trigger eczema flare-ups.
Environmental Triggers
Environmental factors play a crucial role in triggering eczema symptoms, including those affecting the scalp. Common environmental triggers for scalp eczema include:
1. Harsh Hair Care Products: Shampoos, conditioners, and styling products containing fragrances, sulfates, and other harsh chemicals can strip the scalp of its natural oils, leading to dryness and irritation.
Weather Conditions: Cold, dry weather can exacerbate scalp eczema symptoms by further drying out the skin, while hot, humid conditions may increase sweating and irritation.
2. Allergens: Exposure to allergens such as pollen, dust mites, and pet dander can trigger immune responses in susceptible individuals, leading to eczema flare-ups on the scalp.
3. Stress: Psychological stress can exacerbate eczema symptoms by disrupting immune function and increasing inflammation. Stress management techniques may help reduce the frequency and severity of scalp eczema flare-ups.
4. Microbial Infections: Fungal or bacterial infections of the scalp can exacerbate eczema symptoms, leading to increased itching, redness, and inflammation. Proper hygiene and antimicrobial treatments may be necessary to manage these infections effectively.
Skin Barrier Dysfunction
The skin barrier plays a critical role in protecting against environmental irritants and retaining moisture. In individuals with eczema, the skin barrier is compromised, allowing irritants to penetrate more easily and moisture to escape, leading to dryness, inflammation, and itching. Disruption of the skin barrier on the scalp can contribute to the development and exacerbation of eczema symptoms in this area.
Diagnosis and Management
Diagnosing eczema on the scalp typically involves a thorough physical examination by a dermatologist, who may also perform patch testing to identify specific allergens or irritants triggering symptoms. Once diagnosed, the management of scalp eczema typically involves a multifaceted approach aimed at reducing inflammation, relieving itching, and restoring the skin barrier. Treatment options may include:
1. Topical Steroids: Topical corticosteroids are commonly prescribed to reduce inflammation and itching associated with scalp eczema. These medications help alleviate symptoms during flare-ups but should be used sparingly to avoid thinning the skin and other side effects.
2. Emollients: Moisturizing creams and ointments help hydrate the skin and restore the damaged skin barrier. Regular use of emollients can help prevent dryness and reduce the frequency of eczema flare-ups on the scalp.
3. Antihistamines: Oral antihistamines may be prescribed to help relieve itching and improve sleep quality in individuals with scalp eczema.
4. Avoidance of Triggers: Identifying and avoiding triggers such as harsh hair care products, allergens, and environmental pollutants can help reduce the frequency and severity of scalp eczema flare-ups.
Stress Management: Stress-reduction techniques such as mindfulness meditation, yoga, and deep breathing exercises may help reduce the impact of psychological stress on scalp eczema symptoms.
Conclusion
Eczema on the scalp presents unique challenges for individuals grappling with this chronic inflammatory skin condition. Understanding the complex interplay of genetic, immunological, environmental, and microbial factors contributing to scalp eczema is essential in devising effective management strategies. By addressing underlying inflammation, restoring the skin barrier, and avoiding triggers, individuals with scalp eczema can achieve better symptom control and improve their quality of life. Early diagnosis and personalized treatment plans tailored to the individual’s specific needs are crucial in managing scalp eczema effectively.