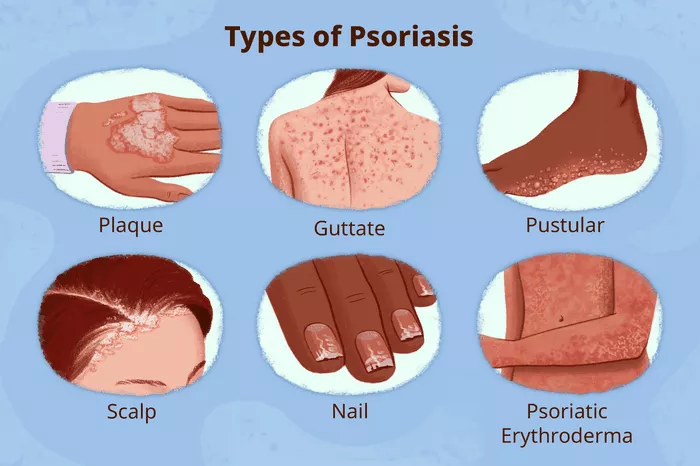
Psoriasis is a chronic autoimmune condition characterized by the rapid buildup of skin cells, leading to the formation of red, scaly patches. Among the various types of psoriasis, one stands out as the most prevalent: plaque psoriasis. Understanding this common form of the condition is crucial for both patients and healthcare professionals alike.
What is Plaque Psoriasis?
Plaque psoriasis, also known as psoriasis vulgaris, is the most prevalent form of psoriasis, affecting approximately 80-90% of individuals diagnosed with the condition. It presents as raised, inflamed patches of skin covered with silvery-white scales, often appearing on the elbows, knees, scalp, and lower back. These patches, or plaques, can vary in size and severity, causing discomfort, itchiness, and sometimes pain for those affected.
Pathophysiology of Plaque Psoriasis
The underlying mechanism of plaque psoriasis involves an abnormal immune response, specifically an overactivation of T cells, a type of white blood cell, within the immune system. In a healthy individual, T cells help protect the body against infections. However, in people with psoriasis, these cells become hyperactive, triggering inflammation and prompting the rapid turnover of skin cells.
This accelerated skin cell turnover cycle leads to the accumulation of cells on the skin’s surface, forming the characteristic plaques associated with psoriasis. Additionally, there is evidence to suggest that genetic factors play a role in predisposing individuals to plaque psoriasis, although environmental triggers such as stress, infections, and certain medications can exacerbate symptoms.
Clinical Presentation and Diagnosis
Diagnosing plaque psoriasis typically involves a thorough examination of the affected skin by a dermatologist or healthcare professional. The presence of raised, red patches covered with silver scales is often indicative of the condition. In some cases, a skin biopsy may be performed to confirm the diagnosis and rule out other skin disorders.
Furthermore, healthcare providers may inquire about a patient’s medical history and family history of psoriasis, as well as any recent stressors or illnesses that may have triggered the onset of symptoms. While there is no definitive cure for plaque psoriasis, various treatment options are available to help manage symptoms and improve quality of life.
Treatment Approaches
Treatment for plaque psoriasis aims to alleviate symptoms, reduce inflammation, and slow down the excessive growth of skin cells. The choice of treatment depends on the severity of the condition, as well as individual factors such as age, overall health, and treatment preferences. Some common treatment approaches include:
1. Topical Therapies: These include corticosteroids, vitamin D analogs, retinoids, and calcineurin inhibitors, which are applied directly to the skin to reduce inflammation and promote healing of the plaques.
2. Phototherapy: Also known as light therapy, this treatment involves exposing the skin to ultraviolet (UV) light under medical supervision. UVB phototherapy and PUVA (psoralen plus ultraviolet A) are two types of phototherapy commonly used to treat plaque psoriasis.
3. Systemic Medications: For more severe cases of plaque psoriasis that do not respond to topical treatments or phototherapy, systemic medications such as methotrexate, cyclosporine, and biologic agents may be prescribed. These medications work by targeting specific components of the immune system involved in the development of psoriasis.
4. Lifestyle Modifications: In addition to medical treatments, adopting certain lifestyle changes can help manage psoriasis symptoms. This includes avoiding triggers such as stress, smoking, and excessive alcohol consumption, as well as practicing good skincare habits and maintaining a healthy diet and weight.
Challenges and Outlook
While treatment options for plaque psoriasis have advanced significantly in recent years, managing the condition can still pose challenges for patients and healthcare providers alike. The chronic nature of psoriasis means that ongoing treatment and monitoring are often necessary to control symptoms and prevent flare-ups.
Furthermore, individuals living with plaque psoriasis may experience physical discomfort, embarrassment, and psychological distress due to the visible nature of the condition. As such, providing comprehensive care that addresses both the physical and emotional aspects of psoriasis is essential for improving patients’ overall well-being.
Looking ahead, ongoing research efforts aimed at better understanding the underlying mechanisms of psoriasis and developing more targeted therapies offer hope for continued advancements in the field. By working collaboratively, healthcare professionals, researchers, and advocacy groups can strive to improve outcomes and quality of life for individuals living with plaque psoriasis and other forms of the condition.
Conclusion
Plaque psoriasis is the most common type of psoriasis, characterized by raised, inflamed patches of skin covered with silvery-white scales. While the exact cause of psoriasis remains unclear, it is thought to involve a combination of genetic, immune, and environmental factors. Effective management of plaque psoriasis typically involves a multidisciplinary approach incorporating topical therapies, phototherapy, systemic medications, and lifestyle modifications.
By raising awareness, promoting early diagnosis, and providing comprehensive care, healthcare professionals can help individuals living with plaque psoriasis lead fulfilling lives and minimize the impact of this chronic condition on their overall well-being.