Skin conditions can be both distressing and challenging to manage, particularly when their symptoms overlap or mimic one another. Seborrheic dermatitis and psoriasis are two such dermatological conditions that share similarities in appearance and symptoms, yet they are distinct in their causes, triggers, and treatment approaches. Differentiating between these two conditions is crucial for accurate diagnosis and effective management. In this article, we delve into the intricacies of seborrheic dermatitis and psoriasis, highlighting their differences and similarities to aid in better understanding and management.
Overview of Seborrheic Dermatitis
Seborrheic dermatitis is a common chronic inflammatory skin condition characterized by red, itchy, and flaky skin, typically occurring in areas rich in sebaceous glands, such as the scalp, face, and chest. It often presents with greasy or oily scales and is associated with an overgrowth of a yeast called Malassezia.
Overview of Psoriasis
Psoriasis, on the other hand, is a chronic autoimmune disorder that accelerates the skin cell turnover process, leading to the rapid buildup of cells on the skin’s surface. This results in thick, red patches covered with silvery scales, commonly affecting the elbows, knees, scalp, and lower back. Psoriasis can also affect the nails, causing pitting, discoloration, and thickening.
Clinical Presentation
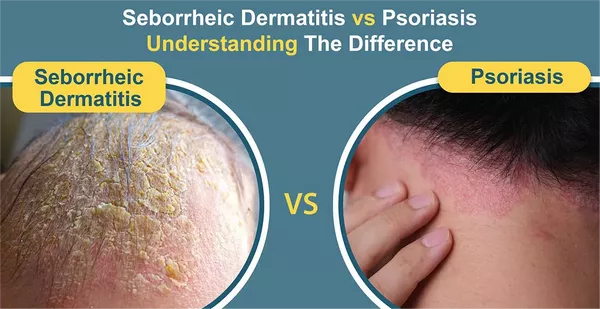
While both seborrheic dermatitis and psoriasis manifest as red, inflamed skin with scales, there are subtle differences in their presentation that aid in distinguishing between the two conditions.
Seborrheic dermatitis typically presents with greasy or oily scales, especially in areas rich in sebaceous glands, such as the scalp, face (particularly the eyebrows, eyelids, and nasolabial folds), and chest. The rash tends to be more diffuse and less well-defined compared to psoriasis lesions.
Psoriasis lesions, on the other hand, are characterized by thick, silvery scales atop well-defined, raised, erythematous plaques. These plaques often have sharp borders and can be symmetrically distributed, commonly affecting the extensor surfaces of the elbows and knees, scalp, and lower back.
Etiology and Pathophysiology
Understanding the underlying mechanisms of seborrheic dermatitis and psoriasis is essential for tailoring appropriate treatment strategies.
Seborrheic dermatitis is believed to result from a combination of genetic predisposition, environmental factors, and an overgrowth of the yeast Malassezia. Factors such as hormonal imbalances, stress, certain medications, and immune system dysfunction may contribute to its development. The exact pathophysiology of seborrheic dermatitis is not fully understood, but it is thought to involve an inflammatory response to Malassezia colonization.
Psoriasis, on the other hand, is primarily an autoimmune disorder characterized by the dysregulation of the immune system, leading to excessive inflammation and aberrant skin cell proliferation. Genetic predisposition plays a significant role in psoriasis, with certain genes, such as those encoding for human leukocyte antigens (HLA), implicated in disease susceptibility. Environmental triggers, such as trauma, infections, stress, and certain medications, can exacerbate psoriasis symptoms by activating the immune system.
Treatment Approaches
Management strategies for seborrheic dermatitis and psoriasis aim to reduce inflammation, alleviate symptoms, and prevent flare-ups. However, due to differences in their underlying causes and pathophysiology, treatment approaches may vary.
For seborrheic dermatitis, treatment often involves topical antifungal agents, such as ketoconazole or ciclopirox, to target the overgrowth of Malassezia. Additionally, topical corticosteroids and calcineurin inhibitors may be prescribed to reduce inflammation and itching. Medicated shampoos containing selenium sulfide, coal tar, or zinc pyrithione are commonly used to control scalp involvement.
Psoriasis management typically involves a multifaceted approach tailored to the severity and extent of the disease. Topical treatments, such as corticosteroids, vitamin D analogs, calcineurin inhibitors, and coal tar preparations, are commonly used for mild to moderate psoriasis. For more severe cases, systemic therapies, including oral retinoids, methotrexate, cyclosporine, or biologic agents targeting specific immune pathways, may be indicated.
Conclusion
Seborrheic dermatitis and psoriasis are two distinct dermatological conditions with overlapping clinical features. While both conditions present with red, inflamed skin and scales, they differ in their underlying causes, triggers, and treatment approaches. Seborrheic dermatitis is associated with an overgrowth of the yeast Malassezia and primarily affects areas rich in sebaceous glands, while psoriasis is an autoimmune disorder characterized by excessive inflammation and aberrant skin cell proliferation. Accurate diagnosis and differentiation between these two conditions are crucial for implementing appropriate treatment strategies and improving patient outcomes. By understanding the nuances of seborrheic dermatitis and psoriasis, healthcare providers can effectively manage these chronic skin conditions and alleviate patients’ symptoms and discomfort.