Vitiligo, a dermatological condition characterized by the loss of skin pigment resulting in white patches, stands as a poignant reminder of the intricate interplay between our immune system and our skin. Beyond its outward appearance, vitiligo’s chronicity underscores the challenges faced by those living with this condition, navigating through periods of stability and progression with no definitive cure in sight.
Defining Vitiligo and Its Chronic Nature
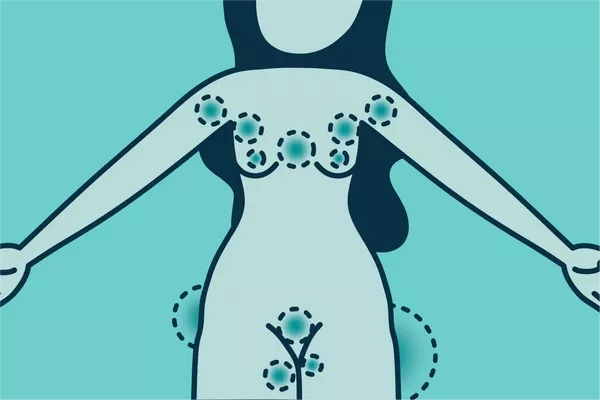
Vitiligo, derived from the Latin word “vitium” meaning “blemish,” manifests as depigmented patches on the skin due to the destruction of melanocytes, the cells responsible for producing melanin, the pigment that gives skin its color. These patches can appear anywhere on the body, including the face, hands, arms, feet, and other areas exposed to the sun.
Central to understanding the chronicity of vitiligo is recognizing its autoimmune nature. In individuals with vitiligo, the immune system mistakenly targets and attacks melanocytes, leading to their destruction. Despite significant advancements in dermatology, there is currently no cure for vitiligo. The chronic nature of the condition means it persists over time, necessitating ongoing management and treatment strategies.
Discussing the Course of Vitiligo
One of the most challenging aspects of vitiligo is its unpredictable course. Individuals may experience periods of stability where the depigmented patches remain unchanged, followed by phases of progression where new patches develop or existing ones expand. This variability can significantly impact the emotional well-being and quality of life of those affected.
Moreover, vitiligo is known for its potential to spread over time, with new patches emerging in previously unaffected areas. While the exact triggers for this spread remain elusive, factors such as stress, trauma to the skin, and certain autoimmune conditions may exacerbate the condition.
Despite its chronicity, there is a glimmer of hope for some individuals with vitiligo. In rare cases, spontaneous repigmentation may occur, wherein melanocytes reappear in depigmented areas, leading to the restoration of skin color. However, this phenomenon is unpredictable and not guaranteed for all individuals with vitiligo.
Treatment Options and Management
While there is no definitive cure for vitiligo, various treatment options aim to manage the condition, slow its progression, and potentially restore some pigment to the affected skin. These treatments range from topical corticosteroids and calcineurin inhibitors to phototherapy and surgical interventions such as skin grafting and melanocyte transplantation.
Topical corticosteroids work by suppressing the immune response in the skin, reducing inflammation, and allowing for repigmentation in some cases. Phototherapy, including narrowband UVB and excimer laser therapy, targets depigmented patches with specific wavelengths of light, stimulating melanocyte activity and promoting repigmentation.
In recent years, emerging therapies such as Janus kinase (JAK) inhibitors have shown promise in treating vitiligo by modulating the immune response and promoting melanocyte regeneration. While these treatments offer hope for individuals with vitiligo, further research is needed to establish their long-term efficacy and safety.
In addition to medical interventions, sun protection plays a crucial role in managing vitiligo. Sunscreen with a high SPF helps protect depigmented skin from sunburn and further damage, as individuals with vitiligo are more susceptible to sunburn and skin cancer.
Addressing Psychological and Emotional Aspects
Beyond its physical manifestations, vitiligo can have a profound impact on an individual’s mental health and emotional well-being. The visible nature of the condition may lead to feelings of self-consciousness, social anxiety, and depression. As such, addressing the psychological aspects of vitiligo is essential in holistic management.
Support groups, counseling services, and online communities provide valuable resources for individuals seeking emotional support and coping strategies for living with vitiligo. Encouraging self-acceptance and promoting body positivity can empower individuals to embrace their unique beauty and overcome societal stigmas associated with skin conditions.
Additional Resources and Information
For those seeking further information and support regarding vitiligo, reputable sources such as medical organizations, vitiligo foundations, and research institutions offer a wealth of resources. These include educational materials, research updates, and opportunities to participate in clinical trials exploring novel treatments for vitiligo.
FAQs addressing common concerns and questions about vitiligo can help individuals better understand their condition and make informed decisions about their treatment journey. Additionally, a glossary of relevant medical terms provides clarity on terminology commonly used in discussions about vitiligo and dermatological conditions.
Conclusion
In conclusion, vitiligo’s chronic nature underscores the importance of comprehensive management strategies aimed at addressing both its physical and emotional aspects. By fostering a deeper understanding of the condition and promoting empathy and support within our communities, we can strive to improve the quality of life for individuals living with vitiligo.