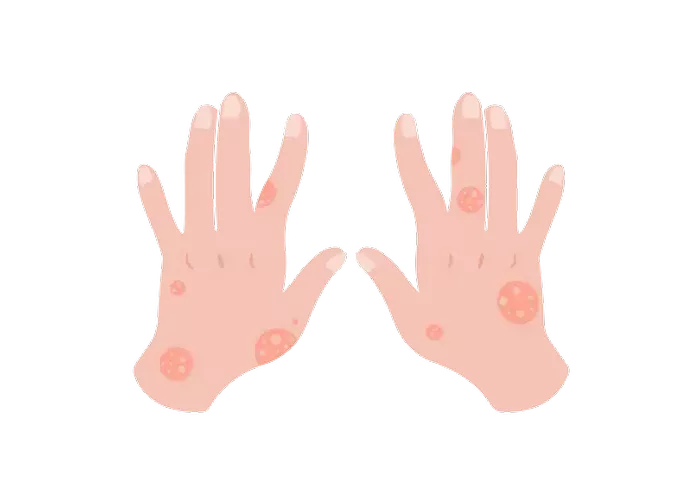
Autoimmune urticaria, also known as chronic spontaneous urticaria (CSU), presents a perplexing challenge for both patients and healthcare providers. Characterized by the sudden onset of hives or wheals that persist for more than six weeks, this condition significantly impacts the quality of life of affected individuals. While the triggers for acute urticaria may be easier to identify, the etiology of autoimmune urticaria often remains elusive, leading to frustration and prolonged suffering. In this article, we delve into the intricate mechanisms behind autoimmune urticaria, exploring the various factors that contribute to its onset and persistence.
Understanding Autoimmune Urticaria: A Complex Interplay
Autoimmune urticaria is a multifactorial disorder involving intricate interactions between genetic predisposition, immune dysregulation, and environmental triggers. While the exact cause remains uncertain in many cases, researchers have identified several key factors that contribute to the development of this condition.
Immune Dysregulation: The Core of Autoimmune Urticaria
Central to the pathogenesis of autoimmune urticaria is immune dysregulation, where the body’s immune system mistakenly targets its own tissues, leading to inflammation and tissue damage. In the case of autoimmune urticaria, autoantibodies against various components of the skin, particularly IgE and IgG antibodies, play a pivotal role.
Research suggests that circulating autoantibodies, such as anti-IgE and anti-FcεRI antibodies, can bind to mast cells and basophils, triggering the release of histamine and other inflammatory mediators. This immune activation results in the characteristic symptoms of urticaria, including itching, redness, and swelling.
Genetic Predisposition: Unraveling the Genetic Puzzle
While autoimmune urticaria is not strictly inherited, there appears to be a genetic predisposition that influences an individual’s susceptibility to the condition. Genome-wide association studies (GWAS) have identified several genetic variants associated with an increased risk of developing autoimmune urticaria.
One such variant is located within the human leukocyte antigen (HLA) region, which plays a crucial role in the immune response by presenting antigens to T cells. Variations in HLA genes may affect immune function and contribute to the development of autoimmune disorders, including urticaria.
Environmental Triggers: Unmasking the Culprits
In addition to genetic factors, environmental triggers can also precipitate or exacerbate autoimmune urticaria in susceptible individuals. These triggers vary widely and may include:
1. Infections: Viral or bacterial infections can stimulate the immune system and trigger an autoimmune response, leading to the onset of urticaria. Common culprits include upper respiratory infections, urinary tract infections, and viral hepatitis.
2. Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and ACE inhibitors, have been implicated in the development of urticaria. Drug-induced urticaria may occur through direct immune activation or non-immunologic mechanisms.
3. Stress: Psychological stress can exacerbate existing autoimmune conditions, including urticaria. Stress triggers the release of cortisol and other stress hormones, which can modulate immune function and increase inflammation, potentially worsening urticarial symptoms.
4. Dietary Factors: While rare, certain foods or food additives may trigger autoimmune urticaria in sensitive individuals. Common culprits include shellfish, eggs, nuts, and food additives such as sulfites and food dyes.
5. Autoimmune Disorders: Autoimmune urticaria is often associated with other autoimmune conditions, such as thyroid disorders, rheumatoid arthritis, and systemic lupus erythematosus. The presence of these comorbidities may indicate a shared underlying autoimmune mechanism.
The Role of Mast Cells: Gatekeepers of Inflammation
Mast cells are immune cells found throughout the body, particularly in the skin and mucous membranes, where they act as sentinels of the immune system. Upon activation by allergens, pathogens, or autoantibodies, mast cells release a cascade of inflammatory mediators, including histamine, leukotrienes, and cytokines, which promote vasodilation, increased vascular permeability, and tissue swelling characteristic of urticaria.
In autoimmune urticaria, the aberrant activation of mast cells by autoantibodies contributes to the chronic inflammatory response underlying the condition. Strategies aimed at modulating mast cell activity, such as antihistamines, corticosteroids, and biologic agents targeting specific inflammatory pathways, represent promising avenues for the treatment of autoimmune urticaria.
Diagnostic Challenges and Clinical Management
Diagnosing autoimmune urticaria can be challenging due to its heterogeneous presentation and lack of specific diagnostic markers. Healthcare providers rely on clinical history, physical examination, and various laboratory tests to differentiate autoimmune urticaria from other forms of chronic urticaria and identify potential underlying triggers.
Treatment strategies for autoimmune urticaria focus on symptom management and addressing underlying immune dysregulation. First-line therapy typically involves the use of second-generation H1 antihistamines, such as cetirizine or loratadine, which block the effects of histamine and alleviate itching and rash. In cases refractory to antihistamines, additional therapies, including oral corticosteroids, leukotriene receptor antagonists, and biologic agents targeting IgE or IL-5, may be considered.
Conclusion
Autoimmune urticaria represents a multifaceted disorder characterized by immune dysregulation, genetic predisposition, and environmental triggers. While significant progress has been made in understanding the underlying mechanisms driving this condition, many aspects remain incompletely understood.
Moving forward, continued research efforts aimed at elucidating the genetic and immunologic factors contributing to autoimmune urticaria are essential for the development of targeted therapies and personalized treatment approaches. By unraveling the complexities of autoimmune urticaria, we can hope to improve outcomes and quality of life for individuals living with this chronic and often debilitating condition.