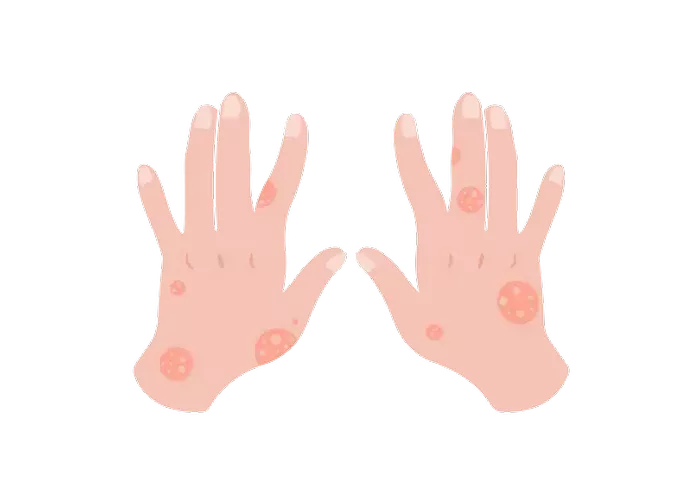
Psoriasis is a chronic autoimmune disease characterized by the rapid growth of skin cells, resulting in the formation of thick, red patches with silvery scales. Despite being a prevalent condition, psoriasis is often misunderstood, with misconceptions leading to stigma and social isolation for those affected. In this article, we delve into the intricacies of psoriasis, from its definition and symptoms to diagnosis, treatment, and strategies for living well with the condition.
Definition and Explanation
Psoriasis is not merely a skin disorder; it is a complex autoimmune disease that affects approximately 2-3% of the global population. The immune system, which normally defends the body against infections and diseases, mistakenly attacks healthy skin cells in individuals with psoriasis. This aberrant immune response speeds up the skin cell turnover process, causing new cells to surface every few days instead of weeks. The accumulation of these excess cells results in the formation of raised, red patches known as plaques.
Several types of psoriasis exist, each with its own distinct characteristics:
1. Plaque Psoriasis: This is the most common form, accounting for about 80% of cases. Plaque psoriasis presents as thick, red patches covered with silvery scales.
2. Guttate Psoriasis: Typically triggered by bacterial infections such as strep throat, guttate psoriasis appears as small, drop-shaped lesions on the trunk, limbs, and scalp.
3. Inverse Psoriasis: Commonly found in skin folds such as the armpits, groin, and under the breasts, inverse psoriasis manifests as smooth, red lesions.
4. Pustular Psoriasis: Characterized by white, pus-filled blisters surrounded by red skin, pustular psoriasis can be localized or widespread.
5. Erythrodermic Psoriasis: The least common but most severe form, erythrodermic psoriasis causes widespread redness and scaling of the skin, often accompanied by severe itching or pain.
Symptoms and Triggers
The symptoms of psoriasis can vary in severity and may include:
- Red patches of skin covered with thick, silvery scales
- Dry, cracked skin that may bleed
- Itching, burning, or soreness
- Nail changes, such as pitting, discoloration, or separation from the nail bed
- Joint pain or swelling, a condition known as psoriatic arthritis
While the exact cause of psoriasis remains unknown, certain factors can trigger or exacerbate symptoms:
- Stress: Emotional stress or trauma can trigger flare-ups or worsen existing symptoms.
- Infections: Streptococcal infections, such as strep throat, can trigger guttate psoriasis in susceptible individuals.
- Skin Injuries: Trauma to the skin, such as cuts, scrapes, or sunburns, may trigger the development of psoriasis lesions, a phenomenon known as the Koebner response.
- Medications: Certain medications, including lithium, antimalarial drugs, and beta-blockers, can exacerbate psoriasis symptoms in some individuals.
Diagnosis and Treatment
Diagnosing psoriasis typically involves a thorough physical examination and medical history review by a dermatologist. In some cases, a skin biopsy may be performed to confirm the diagnosis.
Treatment options for psoriasis aim to alleviate symptoms, reduce inflammation, and slow down the skin cell turnover process. Common treatment modalities include:
1. Topical Treatments: Corticosteroids, vitamin D analogs, retinoids, and coal tar preparations are often used to reduce inflammation and scale formation.
2. Phototherapy (Light Therapy): Exposure to ultraviolet (UV) light can help slow down the rapid growth of skin cells and reduce inflammation.
3. Oral Medications: Systemic medications, such as methotrexate, cyclosporine, and acitretin, may be prescribed for moderate to severe cases of psoriasis.
4. Biologic Therapies: Biologic drugs, which target specific components of the immune system involved in the development of psoriasis, have revolutionized the treatment of moderate to severe psoriasis and psoriatic arthritis.
It’s essential for individuals with psoriasis to work closely with their dermatologist to develop a personalized treatment plan that addresses their specific needs and concerns.
Living with Psoriasis
Living with psoriasis can present various challenges, both physical and emotional. However, with proper management and support, individuals with psoriasis can lead fulfilling lives. Here are some tips for managing psoriasis and reducing flares:
1. Follow a Skincare Routine: Moisturize regularly to prevent dryness and itching, and avoid harsh soaps or skincare products that may irritate the skin.
2. Practice Stress Management: Incorporate stress-reduction techniques such as meditation, yoga, or deep breathing exercises into your daily routine.
3. Maintain a Healthy Lifestyle: Eat a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, and avoid smoking and excessive alcohol consumption.
4. Seek Support: Connect with others who have psoriasis through support groups or online forums, and consider seeking professional help from a therapist or counselor to cope with the emotional impact of the condition.
Conclusion
In conclusion, psoriasis is a chronic autoimmune disease that affects millions of people worldwide. While there is currently no cure for psoriasis, effective treatment options are available to manage symptoms and improve quality of life. By understanding the triggers, seeking appropriate medical care, and adopting healthy lifestyle habits, individuals with psoriasis can take control of their condition and thrive.