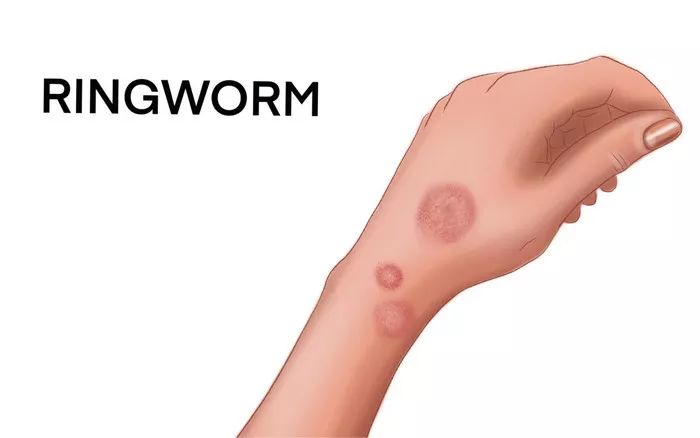
Tinea infections, commonly referred to as ringworm, are superficial fungal infections that affect the skin, hair, and nails. Despite their prevalence, accurate diagnosis can be challenging due to the diverse clinical presentations and overlapping symptoms with other dermatological conditions. Therefore, employing the most effective diagnostic methods is crucial for timely and precise management. In this article, we delve into the intricacies of tinea infection diagnosis, exploring the best practices and advancements in the field.
Understanding Tinea Infections
Tinea infections are caused by dermatophyte fungi, primarily belonging to the genera Trichophyton, Microsporum, and Epidermophyton. These fungi thrive in warm, moist environments and can be transmitted through direct contact with infected individuals or contaminated objects.
Clinical Presentation
The clinical presentation of tinea infections varies depending on the site of infection and the causative organism. Common manifestations include erythematous, scaly lesions with well-defined borders, often accompanied by itching and burning sensations. Tinea corporis presents as circular, erythematous patches on the trunk and limbs, while tinea pedis affects the feet, typically manifesting as interdigital scaling and fissuring. Tinea capitis affects the scalp, leading to hair loss and scaling, whereas tinea cruris affects the groin area, causing pruritic, erythematous plaques. Additionally, tinea unguium, or onychomycosis, affects the nails, resulting in thickening, discoloration, and crumbling.
Challenges in Diagnosis
Diagnosing tinea infections can be challenging due to several factors:
1. Clinical Similarities: The clinical presentation of tinea infections can mimic other dermatological conditions, such as eczema, psoriasis, and bacterial infections, leading to diagnostic confusion.
2. Atypical Presentations: Tinea infections may present atypically, especially in immunocompromised individuals, pediatric patients, and those with chronic medical conditions, necessitating a high index of suspicion.
3. Diagnostic Modalities: Traditional diagnostic methods, such as potassium hydroxide (KOH) preparation and fungal culture, have limitations in terms of sensitivity, specificity, and turnaround time, delaying accurate diagnosis and treatment initiation.
Best Practices for Diagnosis
To overcome the challenges associated with diagnosing tinea infections, healthcare providers should employ a multifaceted approach that combines clinical evaluation, laboratory tests, and emerging diagnostic modalities. The following are the best practices for diagnosing tinea infections:
1. Comprehensive Clinical Assessment: A thorough clinical examination, including history taking and physical examination, is essential for identifying characteristic features of tinea infections. Clinicians should assess the morphology, distribution, and associated symptoms of skin lesions to differentiate tinea from other dermatoses.
2. Dermatoscopy: Dermatoscopy, also known as dermoscopy or epiluminescence microscopy, is a non-invasive technique that allows magnified visualization of skin lesions. Dermatoscopy can aid in identifying subtle features of tinea infections, such as fine scales, erythema, and hair involvement, enhancing diagnostic accuracy.
3. Laboratory Tests: While clinical evaluation provides valuable insights, laboratory tests play a pivotal role in confirming the diagnosis of tinea infections. The following laboratory tests are commonly utilized:
4. Potassium Hydroxide (KOH) Preparation: KOH preparation involves the microscopic examination of skin scrapings treated with 10% KOH solution. KOH dissolves keratinaceous debris, allowing visualization of fungal elements (hyphae and spores) under microscopy. Despite its simplicity and cost-effectiveness, KOH preparation has limitations in terms of sensitivity and specificity, particularly in cases of low fungal burden or non-dermatophyte fungi.
5. Fungal Culture: Fungal culture involves inoculating skin scrapings onto specific culture media and incubating them to promote fungal growth. Culture allows for species identification and antifungal susceptibility testing, aiding in tailored treatment selection. However, fungal culture has a prolonged turnaround time (up to 4 weeks) and may yield false-negative results in patients receiving antifungal therapy.
6. Molecular Diagnostics: Molecular diagnostic techniques, such as polymerase chain reaction (PCR) and loop-mediated isothermal amplification (LAMP), offer rapid and sensitive detection of fungal DNA in clinical specimens. These techniques can identify dermatophyte species with high specificity, even in cases of low fungal burden or culture-negative samples. Molecular diagnostics provide valuable adjuncts to traditional methods, particularly in challenging cases and research settings.
7. Wood’s Lamp Examination: Wood’s lamp examination involves illuminating the skin lesions with ultraviolet light (365 nm) to assess fluorescence patterns. Certain dermatophyte species, such as Microsporum canis, exhibit fluorescence under Wood’s lamp, aiding in rapid identification. However, Wood’s lamp examination has limited sensitivity and specificity, and its utility may be restricted to certain dermatophyte species and geographic regions.
8. Histopathological Examination: In cases where clinical and laboratory findings are inconclusive, histopathological examination of skin biopsy specimens may provide additional diagnostic clues. Histopathology reveals characteristic features of tinea infections, such as fungal hyphae invading the stratum corneum and inflammatory infiltrates, supporting the diagnosis.
Emerging Trends and Future Directions
Advancements in diagnostic technology hold promise for enhancing the accuracy and efficiency of tinea infection diagnosis. Novel techniques, such as matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) and deep learning-based image analysis, are being explored for their potential in rapid and automated identification of fungal pathogens. Additionally, point-of-care tests, such as lateral flow assays and smartphone-based applications, are being developed for decentralized diagnosis, particularly in resource-limited settings.
Conclusion
Diagnosing tinea infections requires a systematic approach that integrates clinical assessment, laboratory tests, and emerging diagnostic modalities. By employing the best practices outlined in this article, healthcare providers can achieve accurate and timely diagnosis, facilitating prompt initiation of appropriate antifungal therapy and preventing complications. As technology continues to evolve, the landscape of tinea infection diagnosis is poised for transformation, promising improved patient outcomes and enhanced disease control.