Hives, medically termed urticaria, represent a prevalent dermatological condition characterized by the sudden appearance of raised, red, and itchy welts on the skin. While hives can arise from various triggers, including allergens, infections, and stress, one often overlooked instigator is medication. Indeed, certain drugs have the potential to induce hives as a side effect, posing discomfort and concern for patients. This article aims to delve deeply into the mechanisms underlying drug-induced hives, explore the diverse array of medications implicated, and elucidate strategies for both management and prevention of this adverse reaction.
Understanding the Complex Mechanisms of Drug-Induced Hives:
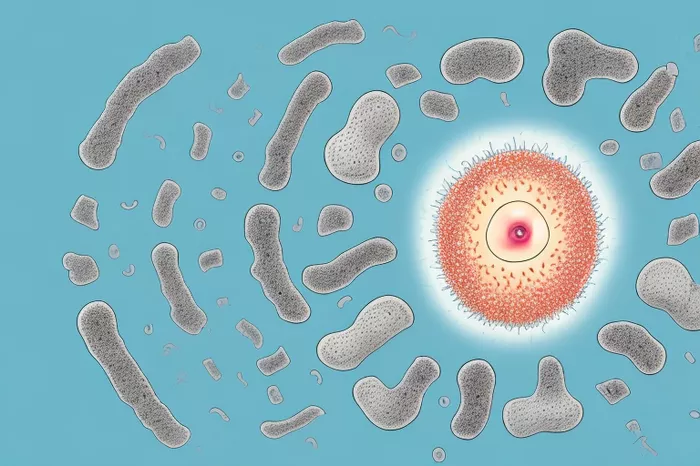
To comprehend the intricate interplay between medications and hives, it is imperative to dissect the underlying mechanisms. Drugs can trigger hives through several pathways, often involving the immune system’s aberrant response. Hypersensitivity reactions, particularly type I hypersensitivity reactions, play a pivotal role in the onset of drug-induced hives. In these reactions, the immune system misidentifies the medication as a threat, leading to the production of antibodies known as immunoglobulin E (IgE). Subsequent exposure to the drug triggers the release of histamine and other inflammatory mediators from mast cells and basophils, culminating in the characteristic symptoms of hives.
Furthermore, certain drugs possess the inherent capability to directly stimulate mast cells, independent of IgE-mediated mechanisms. These drugs, termed mast cell degranulators, prompt the rapid release of histamine, prostaglandins, and leukotrienes, thereby instigating an inflammatory cascade within the skin. Additionally, medications may disrupt the delicate balance of immune cells within the skin, fostering a pro-inflammatory milieu conducive to the development of hives.
The repertoire of medications implicated in drug-induced hives spans across diverse therapeutic classes, each harboring unique mechanisms of action and adverse effect profiles. Antibiotics, particularly penicillins and sulfonamides, reign supreme among the offenders, eliciting hypersensitivity reactions in susceptible individuals. Nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin and ibuprofen, also occupy a prominent place on the list of culprits, with aspirin sensitivity correlating strongly with the development of hives. Other noteworthy offenders include angiotensin-converting enzyme (ACE) inhibitors, opioids, contrast agents, and biologic therapies, each capable of inciting hives through distinct immunologic or pharmacologic mechanisms.
Navigating the Landscape of Medications Implicated in Drug-Induced Hives:
1. Antibiotics:Antibiotics represent a cornerstone of modern medicine, indispensable in the treatment of bacterial infections. However, their indiscriminate use is often fraught with adverse consequences, including the development of hives. Penicillins, cephalosporins, sulfonamides, and quinolones stand out as notorious triggers of drug-induced hives, underscoring the importance of judicious antibiotic prescribing practices.
2. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):Widely utilized for their analgesic, antipyretic, and anti-inflammatory properties, NSAIDs exert their effects by inhibiting the enzyme cyclooxygenase (COX), thereby impeding the synthesis of pro-inflammatory prostaglandins. However, the benefits of NSAIDs are tempered by their propensity to provoke adverse reactions, including hives. Aspirin, in particular, has garnered attention for its role in precipitating hives, especially in individuals with underlying asthma or aspirin sensitivity.
3. Angiotensin-Converting Enzyme (ACE) Inhibitors:ACE inhibitors represent a cornerstone in the management of hypertension and heart failure, exerting their antihypertensive effects by inhibiting the conversion of angiotensin I to angiotensin II. Despite their efficacy, ACE inhibitors are not immune to adverse effects, with drug-induced hives emerging as a potential complication in susceptible individuals.
4. Opioids:Opioids, prized for their potent analgesic properties, are commonly prescribed for the management of acute and chronic pain. However, their therapeutic utility is offset by the risk of adverse reactions, including hives. Morphine, codeine, and other opioids may provoke hives, albeit less frequently than other drug classes.
5. Contrast Agents:Contrast agents serve as indispensable tools in diagnostic imaging, facilitating the visualization of anatomical structures and pathological processes. However, their administration is occasionally marred by the emergence of adverse reactions, including hives. Iodine-based contrast agents, in particular, have been implicated in precipitating allergic reactions, underscoring the need for vigilant monitoring and prompt intervention.
6. Biologic Therapies:Biologic therapies represent a revolutionary paradigm in the treatment of autoimmune and inflammatory disorders, offering targeted and precise interventions that modulate specific immune pathways. Despite their efficacy, biologic therapies are not devoid of adverse effects, with drug-induced hives emerging as a potential complication in susceptible individuals.
Management Strategies for Drug-Induced Hives:
The management of drug-induced hives hinges on a multifaceted approach encompassing prompt identification, cessation of the offending medication, symptomatic relief, and prevention of recurrence. Upon suspicion of drug-induced hives, a thorough evaluation of the patient’s medication history is imperative, with careful scrutiny of recent drug exposures and temporal relationships with symptom onset. Discontinuation of the offending medication is paramount, accompanied by the initiation of symptomatic therapy to alleviate itching and reduce inflammation.
1. Antihistamines:Antihistamines represent the mainstay of pharmacologic therapy for drug-induced hives, exerting their effects by antagonizing the actions of histamine at H1 receptors. First-generation antihistamines, such as diphenhydramine and hydroxyzine, are prized for their sedative properties and rapid onset of action, making them well-suited for acute symptom relief. In contrast, second-generation antihistamines, including loratadine and cetirizine, offer the advantage of improved tolerability and reduced sedation, making them ideal for long-term management.
2. Corticosteroids:In cases of severe or refractory hives, systemic corticosteroids may be employed to suppress inflammation and modulate immune responses. Oral prednisone is commonly prescribed for short-term use, with gradual tapering to minimize the risk of rebound flares and adrenal suppression. However, the use of corticosteroids is reserved for select cases due to their potential for systemic side effects and long-term complications.
3. Epinephrine:In rare instances of anaphylaxis or severe allergic reactions, prompt administration of epinephrine via intramuscular injection is warranted to reverse bronchoconstriction, vasodilation, and systemic hypotension. Epinephrine acts rapidly to alleviate life-threatening symptoms and stabilize vital signs, underscoring its indispensable role in the acute management of drug-induced hives.
Prevention Strategies for Drug-Induced Hives:
Preventing drug-induced hives necessitates a proactive and vigilant approach, encompassing comprehensive patient assessment, judicious medication prescribing practices, and patient education initiatives. Healthcare providers should conduct a thorough review of the patient’s medical history, including prior allergic reactions, medication intolerances, and underlying medical conditions, before initiating any new drug therapy. Allergy testing may be considered in select cases to identify specific triggers and inform future prescribing decisions.
1. Medication Reconciliation:The implementation of robust medication reconciliation processes is paramount in mitigating the risk of drug-induced hives. Healthcare providers should meticulously review the patient’s medication list during each encounter, paying close attention to recent additions or changes that may precipitate adverse reactions. Furthermore, patients should be empowered to actively participate in medication reconciliation efforts, reporting any new symptoms or concerns promptly.
2. Allergy Assessment:Comprehensive allergy assessments play a pivotal role in identifying patients at heightened risk of drug-induced hives. Healthcare providers should elicit a detailed allergy history from patients, including prior allergic reactions, medication intolerances, and environmental allergens. Skin prick testing and serum-specific IgE assays may be employed to identify specific drug allergens and inform future prescribing decisions.
3. Patient Education:Effective patient education initiatives are essential in fostering medication safety and adherence. Patients should be educated about the signs and symptoms of drug-induced hives, emphasizing the importance of promptly reporting any new or unusual symptoms to their healthcare providers. Furthermore, patients should be counseled on the significance of medication adherence, proper dosing techniques, and the potential consequences of non-compliance.
4. Alternative Therapies:In cases where drug-induced hives pose significant challenges to medication management, consideration may be given to alternative therapies or treatment modalities. Healthcare providers should explore non-pharmacologic interventions, lifestyle modifications, and complementary therapies that may offer symptom relief without exacerbating underlying allergic reactions.
Conclusion:
In conclusion, drug-induced hives represent a complex and multifaceted clinical entity, characterized by the sudden onset of raised, red, and pruritic skin lesions following medication exposure. Understanding the intricate interplay between medications and hives is paramount for healthcare providers to recognize, diagnose, and manage this adverse reaction effectively. By elucidating the underlying mechanisms, exploring the diverse array of medications implicated, and implementing comprehensive management and prevention strategies, healthcare providers can optimize patient care and ensure medication safety. Moving forward, continued research efforts and collaborative initiatives are warranted to advance our understanding of drug-induced hives and improve patient outcomes in clinical practice.
Related Topics: