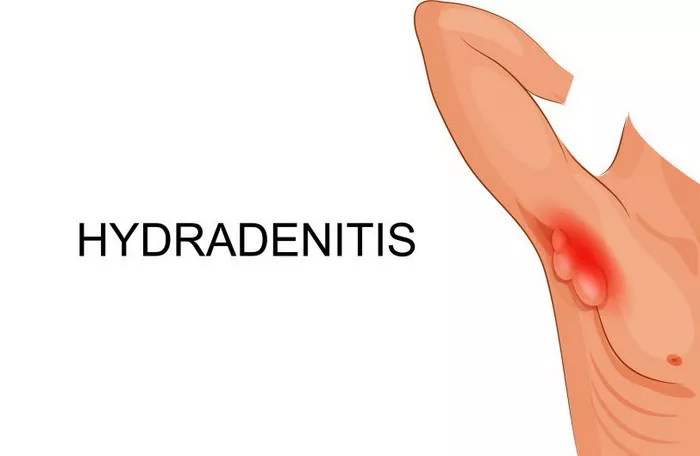
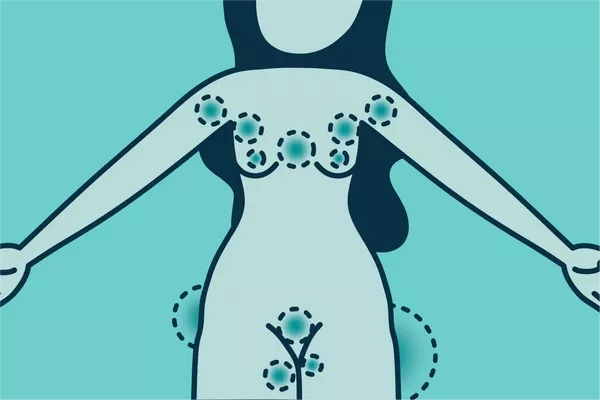
Hidradenitis suppurativa (HS) is a chronic skin condition characterized by painful lumps under the skin that often develop in areas where skin rubs together, such as the armpits, groin, buttocks, and under the breasts. The exact cause of HS is not fully understood, but research has suggested a strong association between smoking and the development and severity of this condition. In this article, we will delve into the relationship between smoking and hidradenitis suppurativa, exploring the potential mechanisms by which smoking may contribute to the onset and progression of this distressing skin disorder.
Understanding Hidradenitis Suppurativa
Before we discuss the role of smoking, it’s essential to grasp the basics of hidradenitis suppurativa. HS is characterized by recurrent, painful nodules and abscesses that can rupture and lead to the formation of sinus tracts beneath the skin. This condition is often associated with inflammation of the hair follicles and sweat glands, primarily affecting areas rich in apocrine glands—the glands responsible for producing sweat.
HS tends to start after puberty and is more common in women than men. The disease’s exact cause is complex, likely involving a combination of genetic, immunological, and environmental factors. Risk factors for HS include obesity, metabolic syndrome, and smoking.
The Link Between Smoking and HS
Several studies have suggested a strong association between smoking and the development of hidradenitis suppurativa. A systematic review published in the Journal of the American Academy of Dermatology concluded that current and former smokers are significantly more likely to develop HS than non-smokers. Another study found that smoking is associated with an earlier onset of HS and more severe disease manifestations.
Potential Mechanisms
The precise mechanisms by which smoking contributes to hidradenitis suppurativa are not entirely understood, but several theories have been proposed:
1. Impact on Immune Function: Smoking is known to have immunomodulatory effects, altering the immune response and impairing the body’s ability to combat infections. In HS, inflammation and immune dysregulation play a crucial role in disease pathogenesis. Smoking-induced immune dysfunction may exacerbate these processes, leading to the development and persistence of HS lesions.
2. Vascular Effects: Smoking is associated with vascular dysfunction, including impaired blood flow and endothelial damage. Poor vascular health can compromise tissue oxygenation and nutrient delivery, potentially contributing to the formation of abscesses and delayed wound healing—hallmarks of HS.
3. Hormonal Influence: Smoking can disrupt hormonal balance, particularly androgen levels. HS is more prevalent in women and is often associated with hormonal changes, suggesting that hormonal factors may influence disease development. Smoking-induced hormonal alterations could contribute to the pathogenesis of HS.
Clinical Observations
Clinical observations further support the link between smoking and hidradenitis suppurativa. Studies have consistently demonstrated that smokers with HS tend to have more extensive disease involvement, higher rates of recurrence, and poorer treatment outcomes compared to non-smokers. Smoking cessation has been associated with disease improvement and reduced severity, highlighting the potential impact of smoking on HS progression.
Public Health Implications
Given the compelling evidence linking smoking to hidradenitis suppurativa, there are important public health implications. Healthcare providers should prioritize smoking cessation interventions for patients with HS, as quitting smoking may not only improve overall health but also help manage the disease more effectively. Moreover, raising awareness about the detrimental effects of smoking on HS could encourage individuals at risk to make informed lifestyle choices.
Conclusion
In summary, while the exact causative relationship between smoking and hidradenitis suppurativa remains to be fully elucidated, existing evidence strongly suggests that smoking is a significant risk factor for the development and exacerbation of this debilitating skin condition. The mechanisms likely involve a complex interplay of immune dysfunction, vascular impairment, and hormonal changes induced by smoking.
Moving forward, further research is needed to deepen our understanding of these mechanisms and explore targeted interventions aimed at mitigating the impact of smoking on hidradenitis suppurativa. In the clinical setting, smoking cessation should be emphasized as an essential component of HS management, alongside conventional therapies. By addressing modifiable risk factors such as smoking, we can potentially improve outcomes and quality of life for individuals living with hidradenitis suppurativa.
Related Topics: