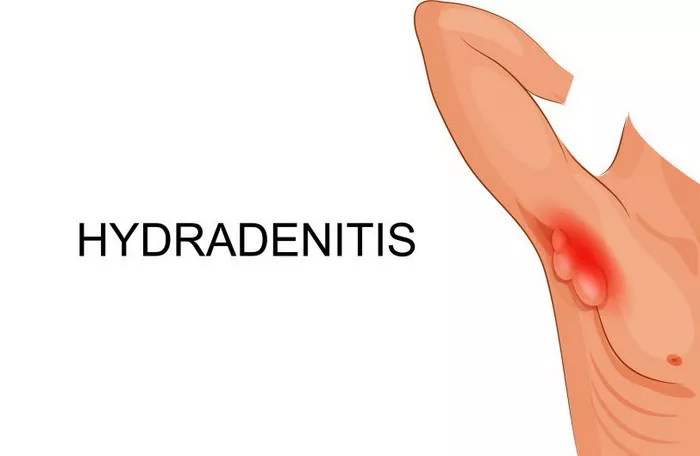
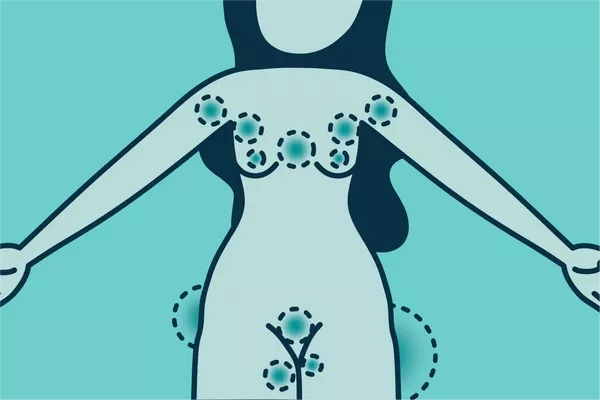
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by painful nodules, abscesses, and sinus tracts predominantly affecting the intertriginous areas of the body such as the axillae, groin, and buttocks. While the hallmark symptoms of HS are pain, swelling, and recurrent abscess formation, itching, or pruritus, is also commonly reported by patients. The sensation of itch in HS can be distressing and significantly impact a patient’s quality of life. Despite its prevalence, the exact mechanisms behind why HS itches remain elusive and require a nuanced exploration.
The Enigma of Pruritus in Hidradenitis Suppurativa
Pruritus, or itching, is a complex sensory perception mediated by the nervous system. It is known to arise from various dermatological conditions, often secondary to inflammation or nerve stimulation. In the context of HS, pruritus presents an intriguing puzzle. Unlike other hallmark symptoms of the disease, such as pain and suppuration, itching in HS lacks a straightforward explanation.
Inflammation and Nerve Interactions
One plausible theory revolves around the role of inflammation and its interaction with nerve fibers. In HS, chronic inflammation within affected skin regions likely sensitizes local nerve endings. This inflammatory milieu can trigger the release of neuropeptides and other chemical mediators that heighten nerve sensitivity, culminating in the perception of itchiness. Moreover, damaged and inflamed tissue in HS may release histamine and other pruritogenic substances, further exacerbating the sensation of itch.
Microbial Factors and Itch Perception
Another avenue of investigation concerns the role of microbial colonization in HS. The disease is associated with overgrowth of bacteria such as Staphylococcus aureus, which can provoke immune responses and contribute to ongoing inflammation. Interestingly, certain bacterial species are known to produce molecules that directly stimulate nerve endings, potentially triggering pruritus. Additionally, the breakdown products of bacterial metabolism might activate specific receptors on sensory nerves, leading to the sensation of itch.
Neuroimmune Crosstalk in HS
Hidradenitis suppurativa is increasingly recognized as a disease involving dysregulation of both the immune system and the nervous system. This neuroimmune crosstalk could hold important clues to the origin of pruritus in HS. Aberrant signaling between immune cells and nerve fibers within affected skin regions may amplify sensory perceptions like itchiness. Factors such as tumor necrosis factor-alpha (TNF-α), interleukins, and nerve growth factor (NGF) have been implicated in this interplay, with potential implications for pruritus.
Impact of Psychological Factors
The experience of chronic pruritus in HS cannot be divorced from its psychological impact. Itching, particularly when persistent, can evoke feelings of frustration, anxiety, and even depression in affected individuals. The interplay between psychological distress and itch perception forms a complex feedback loop that can exacerbate the overall burden of the disease. Addressing these psychological aspects is crucial in managing HS comprehensively.
Clinical Implications and Therapeutic Considerations
Understanding the underlying mechanisms of pruritus in HS is pivotal for developing effective therapeutic strategies. While treatments such as topical corticosteroids and oral antibiotics may alleviate inflammation and reduce itching to some extent, they often fall short of providing long-lasting relief. Novel approaches targeting specific neuroimmune pathways implicated in HS-associated pruritus are currently under investigation. Biologic agents targeting TNF-α and NGF show promise in clinical trials, offering hope for more targeted and effective itch management.
Patient-Centered Care and Future Directions
In the realm of HS management, patient-centered care remains paramount. Acknowledging and addressing the multifaceted impact of pruritus on quality of life is crucial. Clinicians must adopt a holistic approach that integrates symptomatic relief with psychosocial support. Moreover, continued research into the pathophysiology of pruritus in HS is needed to unravel its complexities fully.
Conclusion
In conclusion, pruritus in hidradenitis suppurativa is a vexing symptom with far-reaching implications. While its exact origins remain incompletely understood, emerging evidence points towards a multifactorial interplay involving inflammation, microbial factors, neuroimmune dysregulation, and psychological influences. By elucidating these mechanisms, clinicians and researchers can pave the way for more targeted and effective interventions, ultimately improving the lives of individuals grappling with this challenging disease.
Related Topics: