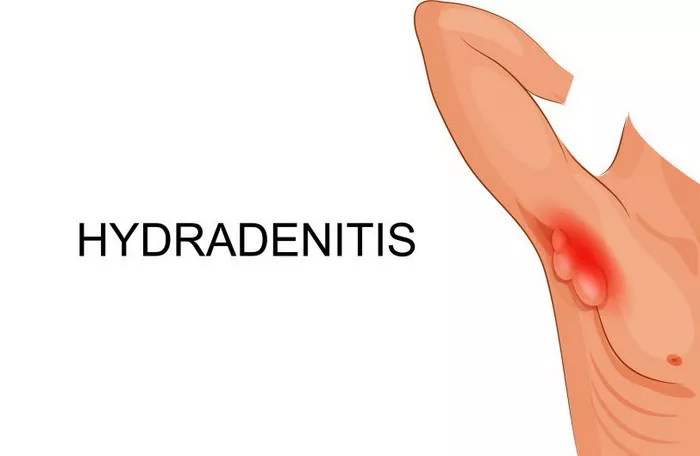
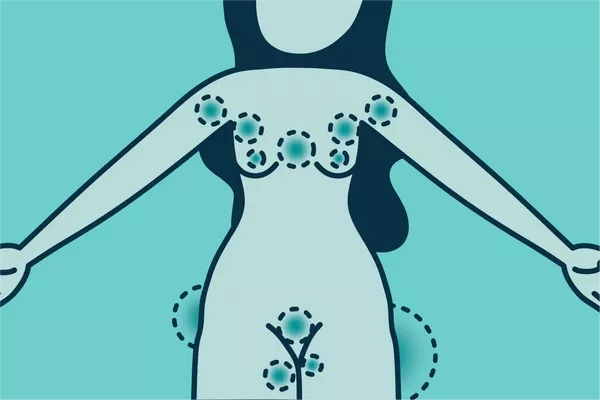
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by painful, recurrent nodules, abscesses, and sinus tracts typically affecting the areas around hair follicles and sweat glands, such as the axillae, groin, and buttocks. This debilitating disease can significantly impact patients’ quality of life due to pain, scarring, and recurrent flare-ups. While there is no definitive cure for HS, surgical intervention is often considered in severe cases where other treatments have failed to provide relief. However, the question remains: can surgery effectively cure HS?
Understanding Hidradenitis Suppurativa
To evaluate the role of surgery in managing HS, it is essential to grasp the nature of the disease. HS is thought to involve a complex interplay of genetic, immune, and environmental factors. It is characterized by recurrent inflammation of hair follicles, leading to the formation of painful nodules and abscesses. Over time, chronic inflammation can result in the formation of sinus tracts and scarring.
HS is typically classified based on severity into Hurley stages:
- Stage I: Single or multiple abscess formation without scarring or sinus tracts
- Stage II: Recurrent abscesses with sinus tracts and scarring
- Stage III: Widespread involvement with multiple interconnected sinus tracts and scarring
Treatment options for HS vary depending on disease severity and can include lifestyle modifications, topical or systemic medications (e.g., antibiotics, retinoids, immunosuppressants), biologics, and surgical interventions.
Role of Surgery in HS Management
Surgery is often considered in HS patients with severe, refractory disease, particularly in those with Hurley stage II and III disease. The goals of surgical intervention in HS include:
- Abscess drainage and debridement: Incision and drainage of acute abscesses to alleviate pain and prevent further progression.
- Excision of affected tissue: Removal of diseased skin and subcutaneous tissue to eliminate affected areas and reduce recurrence.
- Wide excision with skin reconstruction: Radical excision of affected tissue followed by skin grafting or flap reconstruction to manage extensive disease and improve outcomes.
Types of Surgical Procedures
Several surgical procedures can be employed in the management of HS, depending on disease severity and location. These include:
1. Incision and Drainage (I&D): This is a common procedure for acute abscesses in HS. It involves making an incision to drain pus and relieve pressure, providing symptomatic relief. However, I&D alone does not prevent recurrence.
2. Wide Local Excision: In cases of chronic or severe disease, wide excision of affected tissue may be performed to remove diseased areas entirely. This approach aims to eliminate affected tissue and sinus tracts.
3. Laser Therapy: Carbon dioxide (CO2) laser therapy has been explored as an option to vaporize affected tissue and sinus tracts. However, evidence supporting its long-term efficacy is limited.
4. Skin Grafting and Flap Reconstruction: Following extensive excision, skin grafting or flap reconstruction may be necessary to cover the defect and promote wound healing. This approach is reserved for severe or recurrent cases.
Efficacy of Surgery in HS
While surgical intervention can provide significant symptomatic relief and improve quality of life in selected patients with HS, it is important to note that surgery alone may not constitute a cure. Several factors influence the outcomes of surgical procedures for HS:
1. Disease Severity: Surgical outcomes are generally better in patients with localized or early-stage disease compared to those with widespread involvement and scarring.
2. Recurrence Rates: Despite aggressive surgical intervention, HS has a high recurrence rate. New lesions may develop in previously unaffected areas, necessitating ongoing management.
3. Combination Therapy: Surgery is often combined with other treatment modalities such as medical management and lifestyle modifications to optimize outcomes and reduce recurrence.
Conclusion:
In conclusion, while surgery plays a crucial role in the management of severe or refractory HS, it is not a definitive cure. Surgical intervention aims to alleviate symptoms, remove affected tissue, and improve quality of life. However, long-term management of HS requires a multidisciplinary approach involving dermatologists, surgeons, and other healthcare providers.
Future research should focus on identifying novel therapeutic targets and treatment strategies to achieve better outcomes in HS management. Until then, a tailored approach combining surgery with medical therapy remains the cornerstone of managing this challenging disease.
Related Topics: