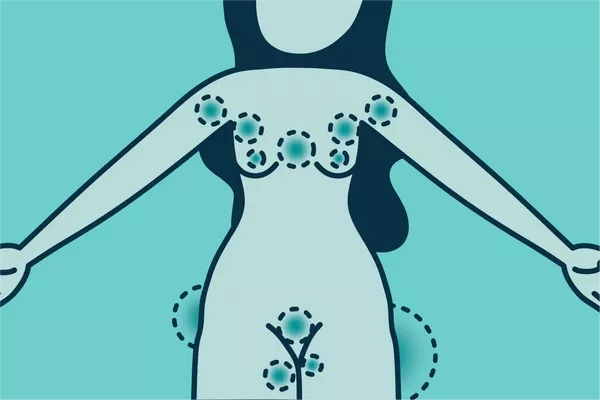
Chronic hives, also known as chronic urticaria, can be an incredibly frustrating and perplexing condition for those who suffer from it. Characterized by recurrent episodes of raised, itchy welts on the skin, chronic hives can significantly impact one’s quality of life and overall well-being. While acute hives typically resolve within a few hours or days, chronic hives persist for six weeks or more, often causing distress and discomfort. In this article, we delve into the complex landscape of chronic hives, exploring the various factors that may contribute to its onset and providing insights into effective management strategies.
Understanding Chronic Hives: Unraveling the Mystery
To comprehend chronic hives, it’s essential to grasp the basics of this condition. Hives, medically referred to as urticaria, manifest as raised, red, and often itchy welts on the skin. These welts can vary in size and shape and may appear suddenly, disappearing just as quickly. While acute hives are commonly triggered by allergic reactions to certain foods, medications, or environmental factors, the etiology of chronic hives is more elusive.
Exploring Potential Causes: Unraveling the Complexity
Pinpointing the precise cause of chronic hives can be challenging due to its multifactorial nature. Several factors may contribute to the development and persistence of this condition, including:
1. Autoimmune Disorders: Research suggests that autoimmune mechanisms play a significant role in many cases of chronic hives. In autoimmune urticaria, the body’s immune system mistakenly identifies its tissues as foreign invaders, triggering the release of histamine and other inflammatory substances that lead to the formation of hives.
2. Underlying Infections: Certain infections, such as hepatitis, Epstein-Barr virus (EBV), and Helicobacter pylori (H. pylori) bacteria, have been associated with chronic hives. It is believed that these infections may stimulate the immune system, leading to the development of hives in susceptible individuals.
3. Allergic Reactions: While acute hives are commonly linked to allergic reactions, allergies may also contribute to chronic hives in some cases. Common allergens such as pollen, pet dander, and certain foods may trigger or exacerbate hives in sensitive individuals.
4. Stress and Emotional Factors: Stress, anxiety, and other emotional factors can exacerbate chronic hives in some individuals. The exact mechanisms underlying the relationship between stress and hives are not fully understood, but it is believed that stress may trigger the release of inflammatory substances that exacerbate skin inflammation.
5. Medications and Food Additives: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and blood pressure medications, have been implicated in the development of hives. Additionally, food additives and preservatives, such as sulfites and food dyes, may trigger hives in susceptible individuals.
6. Environmental Factors: Environmental factors, including extreme temperatures, sunlight exposure, and pressure on the skin (such as tight clothing or scratching), can exacerbate chronic hives in some individuals.
Navigating Diagnosis and Treatment: Seeking Relief
Diagnosing chronic hives often involves a thorough evaluation of medical history, symptom presentation, and possible triggers. In some cases, allergy testing, blood tests, or other diagnostic procedures may be recommended to identify underlying causes or contributing factors.
Once diagnosed, the management of chronic hives typically focuses on alleviating symptoms and identifying and avoiding triggers. Treatment strategies may include:
1. Antihistamines: Non-sedating antihistamines are often the first line of treatment for chronic hives. These medications help block the effects of histamine, reducing itching and inflammation associated with hives.
2. Corticosteroids: In severe cases of chronic hives, oral corticosteroids may be prescribed to reduce inflammation and alleviate symptoms. However, long-term use of corticosteroids is generally discouraged due to the risk of side effects.
3. Immunosuppressants: In cases where antihistamines and corticosteroids are ineffective, immunosuppressant medications may be prescribed to modulate the immune response and reduce inflammation.
4. Avoidance of Triggers: Identifying and avoiding triggers, such as certain foods, medications, or environmental factors, can help prevent recurrent episodes of hives.
5. Stress Management: Stress-reduction techniques, such as mindfulness meditation, deep breathing exercises, and yoga, may help alleviate symptoms of chronic hives by reducing stress and promoting relaxation.
6. Therapeutic Approaches: Other therapeutic approaches, such as phototherapy (light therapy), omalizumab (an anti-IgE monoclonal antibody), and cyclosporine (an immunosuppressant), may be considered in refractory cases of chronic hives.
Conclusion
Chronic hives remain a challenging and enigmatic condition, often requiring a comprehensive approach to diagnosis and management. By understanding the potential causes and triggers of chronic hives, healthcare providers can better tailor treatment strategies to address the unique needs of each individual. While chronic hives can be distressing and disruptive, with proper medical care and lifestyle modifications, many individuals can achieve relief from their symptoms and improve their quality of life.
Related Topics: