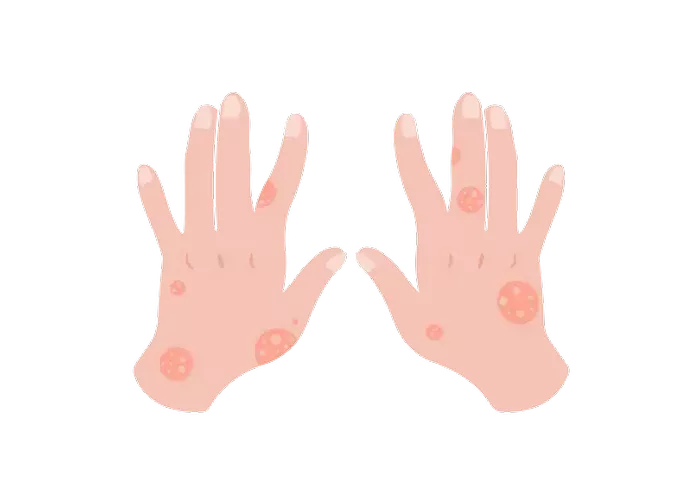
Eczema, also known as atopic dermatitis, is a chronic inflammatory skin condition characterized by itchy, red, and dry patches on the skin. For many, it can be a persistent and painful condition that significantly impacts the quality of life. This article delves into the best practices for managing and treating painful eczema, offering both medical and lifestyle interventions to help individuals find relief and maintain healthy skin.
Understanding Eczema: Causes and Symptoms
Eczema affects millions of people worldwide, and while its exact cause is not entirely understood, it is believed to result from a combination of genetic and environmental factors. The skin condition often runs in families, suggesting a genetic predisposition. Environmental triggers such as allergens, irritants, and stress can exacerbate the symptoms.
Common Symptoms of Eczema
- Itching: Often severe, leading to scratching that can worsen the condition.
- Redness: Inflamed areas that can become swollen and sore.
- Dryness: Skin can become very dry, leading to cracking and bleeding.
- Blisters: In severe cases, blisters may form, which can ooze and crust over.
- Thickened Skin: Prolonged scratching can lead to lichenification, where the skin becomes thick and leathery.
Causes of Eczema
- Genetics: A family history of eczema, asthma, or hay fever increases the likelihood of developing the condition.
- Immune System: An overactive immune response to irritants and allergens.
- Environment: Exposure to pollutants, harsh soaps, and temperature extremes.
- Stress: Psychological stress can exacerbate symptoms.
Diagnosis and Assessment
A healthcare provider typically diagnoses eczema through a physical examination and patient history. In some cases, additional tests such as skin biopsies or allergy tests may be conducted to rule out other conditions and identify specific triggers.
Severity Assessment
Eczema can range from mild to severe, and assessing the severity is crucial for determining the appropriate treatment plan. Healthcare providers may use tools like the Eczema Area and Severity Index (EASI) to evaluate the extent and intensity of the condition.
Medical Treatments for Painful Eczema
Managing painful eczema often requires a multifaceted approach. Medical treatments focus on reducing inflammation, alleviating symptoms, and preventing flare-ups.
Topical Treatments
1. Corticosteroids: These are the most commonly prescribed treatments for reducing inflammation and itching. They vary in strength, from mild over-the-counter options to potent prescription creams.
2. Calcineurin Inhibitors: These non-steroidal creams, such as tacrolimus and pimecrolimus, are effective for sensitive areas like the face and eyelids.
3. Topical PDE4 Inhibitors: Crisaborole is a newer non-steroidal option that helps reduce inflammation and itch.
4. Moisturizers: Emollients and moisturizers are essential for maintaining skin hydration and barrier function. They should be applied regularly, especially after bathing.
Systemic Treatments
For severe eczema that does not respond to topical treatments, systemic medications may be necessary:
1. Oral Corticosteroids: Used for short-term control of severe flare-ups due to their potential side effects with long-term use.
2. Immunosuppressants: Medications like cyclosporine, methotrexate, and azathioprine can help control severe eczema but require close monitoring.
3. Biologics: Dupilumab is a monoclonal antibody approved for treating moderate to severe atopic dermatitis by targeting specific immune pathways involved in eczema.
Phototherapy
Ultraviolet (UV) light therapy can be beneficial for moderate to severe eczema. It helps reduce inflammation and can be an effective option when topical treatments fail. Narrowband UVB is the most commonly used form of phototherapy for eczema.
Antibiotics and Antihistamines
- Antibiotics: If a bacterial infection complicates eczema, antibiotics may be prescribed.
- Antihistamines: These can help manage itching, particularly at night, and improve sleep.
SEE ALSO: What Food Causes Seborrheic Dermatitis
Lifestyle Modifications and Home Remedies
Beyond medical treatments, lifestyle changes and home remedies play a critical role in managing eczema and minimizing flare-ups.
1. Daily Skincare Routine
Maintaining a consistent and gentle skincare routine is vital for managing eczema:
- Bathing: Use lukewarm water and limit baths to 10-15 minutes. Avoid hot water and harsh soaps; instead, use mild, fragrance-free cleansers.
- Moisturizing: Apply a thick layer of moisturizer immediately after bathing to lock in moisture. Choose products with ingredients like ceramides, glycerin, and hyaluronic acid.
- Avoid Scratching: Keep nails short and wear soft gloves at night if scratching during sleep is an issue.
2. Identify and Avoid Triggers
Recognizing and avoiding eczema triggers can help prevent flare-ups:
- Allergens: Common allergens include pollen, pet dander, dust mites, and certain foods.
- Irritants: Avoid harsh soaps, detergents, and fabrics that can irritate the skin. Opt for hypoallergenic and fragrance-free products.
- Stress Management: Incorporate stress-reducing techniques such as yoga, meditation, and deep-breathing exercises.
3. Diet and Nutrition
While no specific diet can cure eczema, certain dietary changes may help manage symptoms:
- Anti-inflammatory Foods: Include foods rich in omega-3 fatty acids, such as salmon, flaxseeds, and walnuts.
- Elimination Diet: Some individuals may benefit from eliminating potential food triggers like dairy, eggs, or gluten.
- Hydration: Drink plenty of water to keep the skin hydrated from within.
4. Natural Remedies
Several natural remedies can provide relief for eczema symptoms, though it’s important to consult with a healthcare provider before trying new treatments:
- Oatmeal Baths: Colloidal oatmeal can soothe itching and inflammation. Add it to bathwater and soak for 15-20 minutes.
- Coconut Oil: Virgin coconut oil has antibacterial properties and can help moisturize the skin.
- Aloe Vera: The gel from the aloe vera plant can soothe and hydrate irritated skin.
Psychological Impact and Support
Living with chronic eczema can take a toll on mental health. The visible nature of the condition, combined with persistent discomfort, can lead to anxiety, depression, and social isolation. Addressing the psychological impact is crucial for comprehensive eczema management.
Support Groups and Counseling
- Support Groups: Joining support groups, either in person or online, can provide a sense of community and shared experiences.
- Counseling: Professional counseling or therapy can help individuals cope with the emotional challenges of living with eczema.
Innovative Treatments and Research
The field of dermatology is continually evolving, with new treatments and research offering hope for better eczema management.
New Medications and Therapies
- Janus Kinase (JAK) Inhibitors: These oral medications are showing promise in treating moderate to severe eczema by targeting specific pathways involved in the inflammatory process.
- Microbiome Research: Emerging studies on the skin microbiome suggest that balancing skin bacteria may play a role in managing eczema. Probiotic and prebiotic treatments are being explored.
Personalized Medicine
Advances in genetic research are paving the way for personalized medicine in eczema treatment. Understanding an individual’s genetic makeup can help tailor treatments to their specific needs, improving efficacy and reducing side effects.
Conclusion
Treating painful eczema requires a comprehensive approach that includes medical treatments, lifestyle modifications, and psychological support. By working closely with healthcare providers and adopting a proactive management strategy, individuals with eczema can significantly reduce symptoms, prevent flare-ups, and improve their quality of life. Continuous research and innovative treatments offer hope for even more effective solutions in the future.
Related Topics: