Ringworm, a common fungal infection also known as dermatophytosis, affects the skin, scalp, and nails. Despite its name, it is not caused by a worm but by fungi called dermatophytes. Characterized by red, itchy, circular rashes with clearer skin in the middle, ringworm can spread through direct contact with infected individuals, animals, or contaminated objects. With the ubiquitous presence of hand sanitizers, especially heightened during the COVID-19 pandemic, a question arises: Can hand sanitizer be used to treat ringworm? This article explores the effectiveness, limitations, and appropriate treatments for ringworm.
Understanding Ringworm
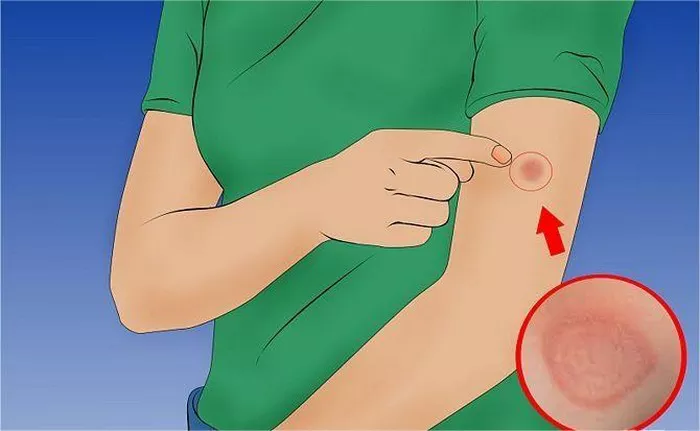
Ringworm is a contagious infection caused by dermatophytes, which thrive on keratin, a protein found in the skin, hair, and nails. It manifests in various forms depending on the body part affected:
- Tinea Corporis: Ringworm of the body
- Tinea Capitis: Ringworm of the scalp
- Tinea Pedis: Athlete’s foot
- Tinea Cruris: Jock itch
- Tinea Unguium: Fungal nail infection
Common symptoms include:
- Circular, red, scaly patches with raised edges
- Itching and discomfort
- Blistering and oozing in severe cases
- Brittle or discolored nails if the nails are infected
The Role of Hand Sanitizers
Hand sanitizers, especially those containing alcohol, are widely recognized for their ability to kill bacteria and some viruses. The active ingredient, usually ethyl or isopropyl alcohol, disrupts the cell membrane of microbes, rendering them inactive. However, the effectiveness of hand sanitizers against fungal infections like ringworm is not as straightforward.
Alcohol and Fungi
Fungi have different cellular structures compared to bacteria and viruses. The outer layer of fungi, composed of a complex cell wall, provides them with greater resilience against environmental factors and disinfectants. Alcohol-based hand sanitizers are less effective against fungi because:
1. Cell Wall Composition: Fungal cell walls contain chitin and glucans, which are less permeable to alcohol. This composition provides a protective barrier that alcohol cannot easily penetrate.
2. Survival Mechanisms: Fungi can produce spores, which are highly resistant to adverse conditions, including alcohol exposure. Spores can survive until they find a suitable environment to grow.
3. Concentration and Contact Time: Even when alcohol can kill fungi, the concentration and duration of exposure needed are higher than those typically provided by hand sanitizers. Most hand sanitizers contain 60-70% alcohol, which is sufficient for bacteria but may not be effective against resilient fungal spores.
SEE ALSO: Does Ringworm Cause Flaky Skin?
Scientific Evidence on Hand Sanitizers and Fungal Infections
Several studies have investigated the efficacy of alcohol-based hand sanitizers against various pathogens. While hand sanitizers are proven to be effective against many bacteria and viruses, their impact on fungi, particularly dermatophytes, remains limited. Research indicates that:
1. Limited Fungicidal Activity: Studies have shown that while alcohol can reduce the number of fungal spores, it does not completely eliminate them. Fungal spores can remain viable even after alcohol exposure, posing a risk of reinfection.
2. Surface Disinfection: Alcohol-based disinfectants can reduce fungal contamination on surfaces, but their effectiveness is contingent on the concentration and exposure time. For instance, a higher alcohol concentration and prolonged contact are necessary to achieve significant fungal reduction.
3. Hand Hygiene: While hand sanitizers can help reduce the transmission of fungi through contaminated hands, they are not a substitute for thorough handwashing with soap and water, which is more effective in removing fungal spores.
Treatment Options for Ringworm
Given the limitations of hand sanitizers, it is crucial to use appropriate treatments for ringworm. Effective management of ringworm involves antifungal medications, which come in various forms:
Topical Antifungal Treatments
For mild to moderate cases of ringworm, topical antifungal creams, ointments, or lotions are commonly prescribed. These treatments are applied directly to the affected area and include:
1. Clotrimazole: Available over-the-counter, clotrimazole is effective against a range of fungal infections. It disrupts the fungal cell membrane, leading to cell death.
2. Miconazole: Another over-the-counter option, miconazole works similarly to clotrimazole and is available in various forms, including creams and powders.
3. Terbinafine: Available both over-the-counter and by prescription, terbinafine is known for its efficacy against dermatophytes. It inhibits the enzyme required for fungal cell wall synthesis.
4. Ketoconazole: Typically prescribed for more severe infections, ketoconazole is available in creams and shampoos for scalp infections.
Oral Antifungal Medications
For more extensive or severe infections, oral antifungal medications may be necessary. These medications require a prescription and include:
1. Terbinafine: In oral form, terbinafine is highly effective for treating nail infections and widespread skin infections. It is taken daily for several weeks to months, depending on the severity.
2. Griseofulvin: An older antifungal medication, griseofulvin is effective but requires a longer treatment duration. It interferes with fungal cell division.
3. Itraconazole: Often prescribed for nail infections, itraconazole is taken in cycles to minimize side effects and enhance efficacy.
Non-Pharmacological Measures
In addition to antifungal medications, several non-pharmacological measures can help manage and prevent ringworm:
1. Hygiene Practices: Regular handwashing with soap and water, especially after touching infected areas or animals, helps prevent the spread of ringworm.
2. Avoiding Shared Items: Personal items such as towels, clothing, and grooming tools should not be shared to prevent cross-contamination.
3. Cleaning and Disinfection: Regular cleaning and disinfection of living spaces, particularly in areas where infected individuals or pets frequent, can reduce fungal spores.
4. Pet Care: Pets can be carriers of ringworm. Ensuring they receive appropriate veterinary care and treatment is essential to prevent human infections.
Conclusion
While hand sanitizers play a crucial role in reducing the spread of many infectious agents, their efficacy against ringworm is limited. The unique structure and resilience of fungi, particularly dermatophytes, require targeted antifungal treatments for effective management. Topical and oral antifungal medications, combined with proper hygiene practices and environmental measures, are essential for treating and preventing ringworm infections.
Relying on hand sanitizers alone is not sufficient to treat ringworm. Individuals experiencing symptoms of ringworm should seek medical advice for appropriate diagnosis and treatment. By understanding the limitations of hand sanitizers and utilizing effective antifungal treatments, individuals can effectively manage and prevent the spread of ringworm, ensuring better skin health and overall well-being.
Related Topics: