Vitiligo is a chronic skin condition characterized by the loss of pigment, resulting in white patches on the skin. While the condition itself is not life-threatening or contagious, it can have profound psychological and social impacts on those affected. One of the most common concerns among individuals diagnosed with vitiligo is whether the condition will spread throughout the body. This article aims to provide a comprehensive understanding of vitiligo’s progression, factors influencing its spread, and available management strategies.
Vitiligo: An Overview
Vitiligo affects approximately 1% of the global population, with no preference for race or gender. It occurs when melanocytes, the cells responsible for producing skin pigment (melanin), are destroyed or malfunction. The exact cause of vitiligo is not fully understood, but it is believed to involve a combination of genetic, autoimmune, and environmental factors.
There are two main types of vitiligo:
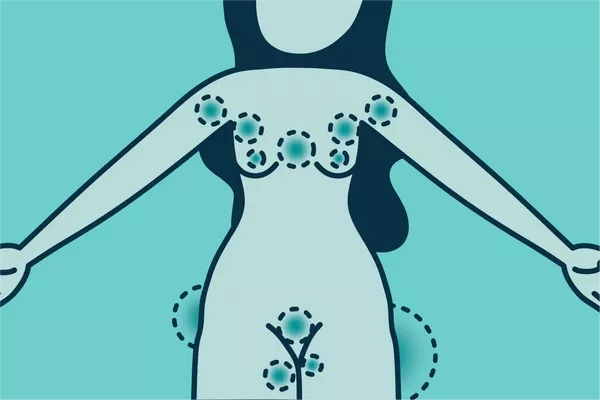
Non-segmental Vitiligo (NSV): This is the most common form and is characterized by symmetrical white patches on both sides of the body. It often starts on the hands, feet, or face.
Segmental Vitiligo (SV): This type is less common and tends to appear on one side of the body. It often begins at a younger age and is more stable, meaning it progresses more slowly than NSV.
Mechanisms of Vitiligo Spread
The spread of vitiligo varies significantly from person to person. Some individuals may experience rapid and widespread loss of pigment, while others might have stable, localized patches for many years. Several factors influence the spread of vitiligo, including genetic predisposition, autoimmune activity, and environmental triggers.
Genetic Factors
Family history plays a significant role in the likelihood of developing vitiligo and its potential spread. Studies have shown that individuals with a family history of vitiligo or other autoimmune diseases are at a higher risk. Genetic research has identified several genes associated with vitiligo, such as NLRP1 and PTPN22, which are involved in immune system regulation. However, possessing these genetic markers does not guarantee the development or spread of vitiligo; it merely increases susceptibility.
Autoimmune Activity
Vitiligo is considered an autoimmune disease, where the body’s immune system mistakenly attacks and destroys melanocytes. This autoimmune activity is believed to be a primary driver of vitiligo’s spread. Inflammatory cytokines and antibodies targeting melanocytes have been detected in the blood of vitiligo patients, indicating ongoing immune system activity. The extent and activity of this autoimmune response can influence how quickly and widely vitiligo spreads.
Environmental and Lifestyle Factors
Environmental factors, such as stress, skin trauma (Koebner phenomenon), and exposure to certain chemicals, can trigger or exacerbate vitiligo. Physical trauma or injury to the skin can lead to the development of new vitiligo patches in affected areas. Additionally, oxidative stress and exposure to ultraviolet (UV) radiation have been implicated in the pathogenesis of vitiligo. Lifestyle factors, including diet, smoking, and overall health, may also impact the condition’s progression.
Patterns of Vitiligo Progression
Vitiligo progression is highly individualistic, with no definitive pattern applicable to all patients. However, some general patterns have been observed:
Localized Vitiligo
In some cases, vitiligo remains localized to a specific area of the body. This pattern is more common in segmental vitiligo but can also occur in non-segmental forms. Localized vitiligo may remain stable for years, with minimal or no spread. Factors contributing to this stability are not entirely understood but may include genetic predisposition and a less active autoimmune response.
Generalized Vitiligo
Generalized vitiligo involves widespread and often symmetrical patches of depigmented skin across various body parts. This pattern is typical of non-segmental vitiligo and tends to progress over time. The rate of spread can vary; some individuals may experience rapid progression, while others see a slow and gradual increase in the affected areas.
Universal Vitiligo
In rare cases, vitiligo can progress to involve nearly the entire body surface, a condition known as universal vitiligo. This extensive depigmentation can have significant psychological and social impacts, as it drastically alters an individual’s appearance. The factors leading to such extensive spread are not fully understood but are likely related to a combination of genetic, autoimmune, and environmental influences.
SEE ALSO: What Is the Cause for Vitiligo
Factors Influencing the Spread of Vitiligo
Understanding the factors that influence vitiligo’s spread is crucial for managing the condition and providing appropriate patient care. Several key factors have been identified:
Age of Onset
The age at which vitiligo begins can influence its progression. Early-onset vitiligo, particularly segmental vitiligo, often stabilizes more quickly than adult-onset non-segmental vitiligo. Children with vitiligo may experience more rapid changes in their condition, necessitating close monitoring and early intervention.
Type of Vitiligo
As mentioned earlier, the type of vitiligo (segmental vs. non-segmental) plays a significant role in its spread. Segmental vitiligo typically progresses more slowly and remains localized, while non-segmental vitiligo is more likely to spread and affect multiple body areas.
Immune System Activity
The activity of the immune system is a critical factor in vitiligo progression. High levels of immune activity, indicated by the presence of specific antibodies and inflammatory markers, can lead to more aggressive and widespread depigmentation. Managing the immune response through medical treatments can help slow the spread.
Skin Trauma
The Koebner phenomenon, where new vitiligo patches develop at sites of skin trauma or injury, highlights the importance of protecting the skin. Avoiding unnecessary skin damage and promptly treating injuries can help minimize the risk of new patches forming.
Psychological Stress
Stress is known to exacerbate many autoimmune conditions, including vitiligo. High-stress levels can trigger or worsen depigmentation. Stress management techniques, such as mindfulness, meditation, and counseling, can be beneficial in managing vitiligo.
Management and Treatment Options
While there is no cure for vitiligo, various treatment options are available to help manage the condition, slow its spread, and improve the appearance of affected skin. Treatment approaches can be categorized into medical therapies, surgical interventions, and lifestyle modifications.
Medical Therapies
1. Topical Corticosteroids: These anti-inflammatory creams can help reduce the immune response and promote repigmentation. They are often used in the early stages of vitiligo or for localized patches.
2 .Topical Calcineurin Inhibitors: Medications like tacrolimus and pimecrolimus can be used as an alternative to corticosteroids, particularly for sensitive areas like the face and neck.
3. Phototherapy: Narrowband UVB (NB-UVB) phototherapy is a common treatment that involves exposing the skin to UVB light, stimulating melanocyte activity and promoting repigmentation.
4. Systemic Therapies: In cases of extensive vitiligo, oral corticosteroids or immunosuppressive drugs may be prescribed to reduce autoimmune activity and slow progression.
5. Excimer Laser: This targeted light therapy can be used to treat small areas of vitiligo, promoting repigmentation with minimal side effects.
Surgical Interventions
1. Skin Grafting: This procedure involves transplanting healthy, pigmented skin to areas affected by vitiligo. It is typically used for stable, localized vitiligo.
2. Melanocyte Transplantation: In this technique, melanocytes are harvested from unaffected skin and transplanted to depigmented areas. This method is still being refined and is not widely available.
Lifestyle Modifications
1. Sun Protection: Protecting the skin from excessive sun exposure is crucial for vitiligo patients. Sunscreen, protective clothing, and avoiding peak UV hours can help prevent further damage and new patch formation.
2. Diet and Nutrition: A balanced diet rich in antioxidants, vitamins, and minerals can support overall skin health. Some studies suggest that certain nutrients, such as vitamin D and folic acid, may benefit vitiligo patients.
3. Stress Management: Incorporating stress-reduction techniques, such as yoga, meditation, and regular exercise, can help manage the psychological impact of vitiligo and potentially slow its progression.
Living with Vitiligo
Vitiligo can significantly impact an individual’s self-esteem and quality of life. Support from healthcare providers, family, and friends is essential in managing the condition’s emotional and psychological aspects. Joining support groups, either in person or online, can provide a sense of community and shared experiences, helping individuals cope with the challenges of living with vitiligo.
Psychological Support
Counseling and therapy can be beneficial for individuals struggling with the emotional impact of vitiligo. Cognitive-behavioral therapy (CBT) and other therapeutic approaches can help build resilience, improve self-esteem, and develop coping strategies.
Cosmetic Camouflage
Many vitiligo patients use cosmetic products to camouflage white patches and even out skin tone. High-quality, long-lasting concealers and makeup can significantly boost confidence and reduce self-consciousness.
Public Awareness and Education
Increasing public awareness and understanding of vitiligo is crucial in reducing stigma and promoting acceptance. Educational campaigns and advocacy efforts can help dispel myths about the condition and support those affected.
Conclusion
Vitiligo is a complex and multifaceted condition with varying patterns of spread and progression. Understanding the factors that influence vitiligo’s spread can help patients and healthcare providers develop effective management strategies. Although there is no cure, a combination of medication and surgical intervention can effectively control the progression of vitiligo.
Related Topics: