Ringworm, also known as dermatophytosis, is a common fungal infection that affects the skin, hair, and nails. Despite its name, it is not caused by a worm but by fungi called dermatophytes. These fungi thrive on keratin, the protein that makes up the outer layer of skin, hair, and nails. While ringworm is typically treated effectively with antifungal medications, understanding its long-term effects is crucial for those affected and healthcare providers.
The Nature of Ringworm
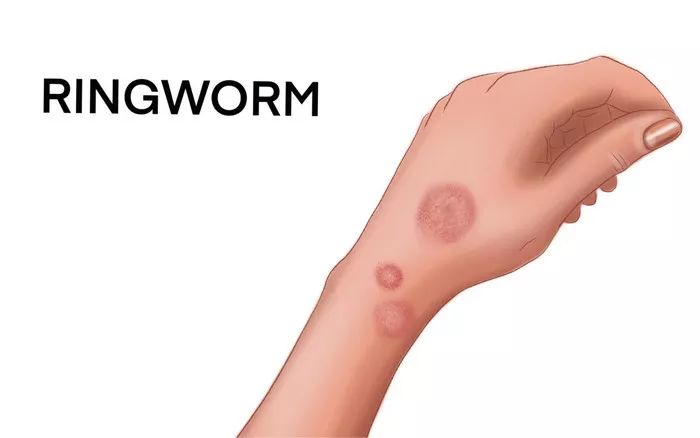
Ringworm can manifest in various parts of the body, leading to different conditions such as tinea pedis (athlete’s foot), tinea corporis (body ringworm), tinea cruris (jock itch), and tinea capitis (scalp ringworm). The infection usually presents as a red, itchy, scaly, and circular rash. When treated promptly, ringworm often resolves without significant long-term consequences. However, if left untreated or in cases of severe infection, there can be notable long-term effects.
Chronic Dermatophytosis
One of the primary long-term effects of ringworm is chronic dermatophytosis, a persistent fungal infection that can recur even after treatment. Chronic dermatophytosis is more common in individuals with compromised immune systems, such as those with HIV/AIDS, diabetes, or other immunosuppressive conditions. This persistent infection can lead to continuous discomfort, itching, and cosmetic concerns. The fungi can adapt to the skin environment, making it challenging to completely eradicate the infection, especially in areas like the nails (onychomycosis) and scalp.
Scarring and Skin Discoloration
Severe or untreated ringworm can cause permanent scarring and discoloration of the skin. The inflammatory response to the infection can lead to changes in skin pigmentation, resulting in hyperpigmentation (dark spots) or hypopigmentation (light spots). These changes are often more noticeable in individuals with darker skin tones and can be a source of psychological distress due to the visible nature of the scars.
Secondary Bacterial Infections
Scratching the itchy, irritated skin caused by ringworm can introduce bacteria into the affected area, leading to secondary bacterial infections. These infections can complicate the clinical picture, requiring additional treatments with antibiotics. In severe cases, secondary infections can cause cellulitis, a deeper skin infection that can spread to the lymph nodes and bloodstream, posing significant health risks.
Hair Loss and Permanent Bald Patches
Ringworm of the scalp (tinea capitis) can lead to hair loss in the infected areas. In severe cases, this can result in permanent bald patches. The inflammation caused by the fungal infection can damage hair follicles, preventing hair from regrowing normally. This condition, known as scarring alopecia, is particularly distressing for children who are more commonly affected by tinea capitis.
Psychological and Social Impact
The visible and often disfiguring nature of ringworm can have a profound psychological impact. Individuals with chronic or severe ringworm may experience reduced self-esteem, anxiety, and depression due to the social stigma associated with visible skin conditions. Children and adolescents, in particular, can face bullying or social exclusion, further exacerbating the emotional toll of the infection.
Increased Susceptibility to Other Infections
Chronic ringworm infections can weaken the skin’s natural barrier, making individuals more susceptible to other infections. The persistent presence of fungi on the skin can create an environment conducive to the colonization and growth of other pathogens. This increased susceptibility can lead to a cycle of recurring infections that are difficult to manage.
Impact on Quality of Life
The persistent itching, discomfort, and cosmetic concerns associated with long-term ringworm can significantly impact an individual’s quality of life. Daily activities may be disrupted, and the constant need for treatment and management of symptoms can be burdensome. Individuals may avoid social interactions or physical activities due to the fear of spreading the infection or due to embarrassment about their appearance.
SEE ALSO: Can I Burn Ringworm Off?
Managing Long-Term Effects
Effective management of ringworm and its long-term effects requires a comprehensive approach that includes medical treatment, lifestyle modifications, and psychological support.
Medical Treatment
For chronic or severe ringworm infections, long-term antifungal therapy may be necessary. This can include oral antifungal medications, which are more effective for deep-seated infections such as those affecting the scalp or nails. Topical antifungal creams and ointments can be used for less severe infections. Regular follow-up with a healthcare provider is essential to monitor the response to treatment and to make necessary adjustments.
Lifestyle Modifications
Maintaining good hygiene and keeping the skin dry are crucial in preventing the recurrence of ringworm. This includes regular hand washing, using antifungal powders in shoes and on the body, and avoiding sharing personal items such as towels, combs, and clothing. Individuals with a history of ringworm should also avoid close contact with infected animals or individuals until the infection is fully resolved.
Psychological Support
Addressing the psychological impact of ringworm is an important aspect of comprehensive care. Counseling or therapy can help individuals cope with the emotional and social challenges associated with chronic skin conditions. Support groups can also provide a sense of community and understanding for those dealing with similar issues.
Conclusion
While ringworm is typically a manageable condition with prompt treatment, understanding its potential long-term effects is crucial for effective management and support. Chronic dermatophytosis, scarring, secondary infections, hair loss, psychological impact, increased susceptibility to other infections, and overall reduced quality of life are significant concerns for those affected by severe or untreated ringworm. A comprehensive approach that includes medical treatment, lifestyle modifications, and psychological support is essential in managing these long-term effects and improving the overall well-being of individuals with ringworm.
Healthcare providers play a vital role in educating patients about the importance of early treatment and prevention strategies to minimize the risk of long-term complications. By raising awareness and providing effective interventions, the long-term impact of ringworm can be significantly reduced, leading to better health outcomes and improved quality of life for those affected.
Related Topics: