Hidradenitis suppurativa (HS) is a chronic skin condition characterized by the formation of painful lumps under the skin, primarily in areas where skin rubs together, such as the armpits, groin, buttocks, and breasts. These lumps can become inflamed and infected, leading to abscesses and tunneling wounds that may exude foul-smelling pus. While pain is a well-documented and debilitating symptom of HS, the question of whether HS is itchy is an important one, as itchiness (pruritus) can significantly affect the quality of life and the management of the condition.
Understanding Hidradenitis Suppurativa
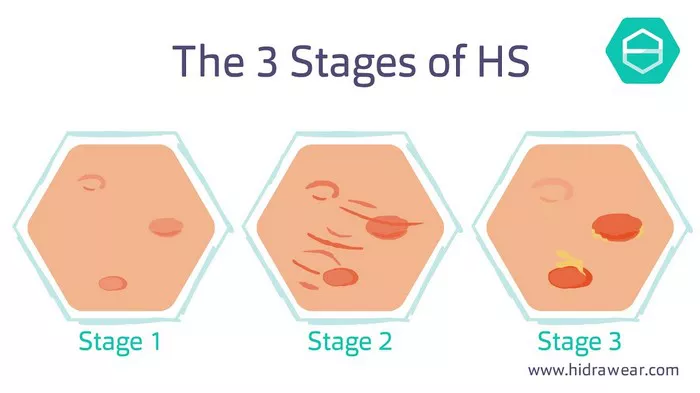
Before delving into the specifics of itchiness in HS, it is crucial to understand the nature of the disease. HS is believed to result from the blockage of hair follicles and subsequent inflammation of the apocrine glands, which are sweat glands located in certain parts of the body. This process leads to the formation of nodules, abscesses, and sinus tracts. The exact cause of HS is not fully understood, but factors such as genetics, hormonal changes, immune system dysfunction, and lifestyle factors (like smoking and obesity) are thought to contribute to its development.
Common Symptoms of Hidradenitis Suppurativa
The primary symptoms of HS include:
1. Painful Nodules and Abscesses: These are the hallmark of HS and can be extremely painful. The nodules can range in size and often become inflamed, leading to abscesses that may rupture and drain pus.
2. Sinus Tracts: Over time, chronic inflammation can lead to the formation of sinus tracts, which are tunnel-like formations under the skin that connect different abscesses. These can be a source of ongoing infection and discomfort.
3. Scarring: Repeated inflammation and healing can result in significant scarring, leading to a puckered or “rope-like” appearance on the skin.
Itchiness in Hidradenitis Suppurativa
While pain is a dominant symptom in HS, itchiness is also a common and often overlooked aspect of the condition. Itchiness can arise from several factors related to HS, including:
1. Inflammation: Chronic inflammation can lead to the release of various inflammatory mediators, such as cytokines and histamines, which can induce itching. The skin around the affected areas may become red, swollen, and itchy as a result.
2. Infection: Secondary bacterial infections, which are common in HS due to the rupturing of abscesses, can cause the skin to become itchy. The presence of bacteria and the body’s immune response to fight the infection can contribute to itching.
3. Healing Process: The healing of wounds and abscesses often involves itching. As new skin forms and repairs the damaged areas, itchiness is a natural part of the healing process. However, in HS, this process is complicated by recurrent inflammation and infection, which can make the itchiness more persistent and severe.
4. Skin Irritation: The use of various topical treatments and dressings to manage HS can sometimes cause skin irritation and allergic reactions, leading to itchiness. Additionally, friction from clothing and sweating can exacerbate skin irritation and itching.
The Impact of Itchiness on Quality of Life
Itchiness in HS can significantly affect a patient’s quality of life. Chronic itching can lead to:
1. Sleep Disturbances: Persistent itching, especially at night, can interfere with sleep, leading to fatigue and affecting overall well-being.
2. Emotional Distress: The constant need to scratch can be distressing and embarrassing, contributing to anxiety, depression, and social isolation.
3. Skin Damage: Frequent scratching can cause further damage to the already compromised skin, leading to increased risk of infection, scarring, and worsening of HS symptoms.
Managing Itchiness in Hidradenitis Suppurativa
Effective management of itchiness in HS involves addressing the underlying causes and providing symptomatic relief. Strategies may include:
1. Anti-Inflammatory Medications: Topical and systemic anti-inflammatory medications can help reduce inflammation and itching. These may include corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and other immunomodulatory agents.
2. Antibiotics: In cases where secondary bacterial infection is present, antibiotics can help control the infection and reduce associated itching.
SEE ALSO: What Does Hidradenitis Suppurativa Smell Like
3. Topical Treatments: Emollients and moisturizers can soothe irritated skin and provide a barrier to protect against further irritation. Medications such as topical corticosteroids and calcineurin inhibitors can also help reduce inflammation and itching.
4. Antihistamines: Oral antihistamines can help control itching by blocking the action of histamines, which are released during inflammatory and allergic reactions.
5. Wound Care: Proper wound care, including the use of appropriate dressings and keeping the affected areas clean, can help reduce skin irritation and itching.
6. Lifestyle Modifications: Avoiding triggers that worsen HS, such as tight clothing, excessive sweating, and smoking, can help manage symptoms, including itchiness.
7. Behavioral Therapies: Cognitive-behavioral therapy (CBT) and other psychological interventions can help patients cope with the emotional and psychological impact of chronic itchiness.
Conclusion
Hidradenitis suppurativa is a complex and chronic skin condition that not only causes painful nodules and abscesses but also significant itchiness. Itchiness in HS can arise from inflammation, infection, the healing process, and skin irritation, and can severely impact a patient’s quality of life. Effective management of itchiness in HS requires a multifaceted approach, including anti-inflammatory and antibiotic treatments, proper wound care, and lifestyle modifications. Addressing itchiness as a key symptom of HS is essential in improving the overall well-being and quality of life of patients living with this challenging condition.
Related Topics: