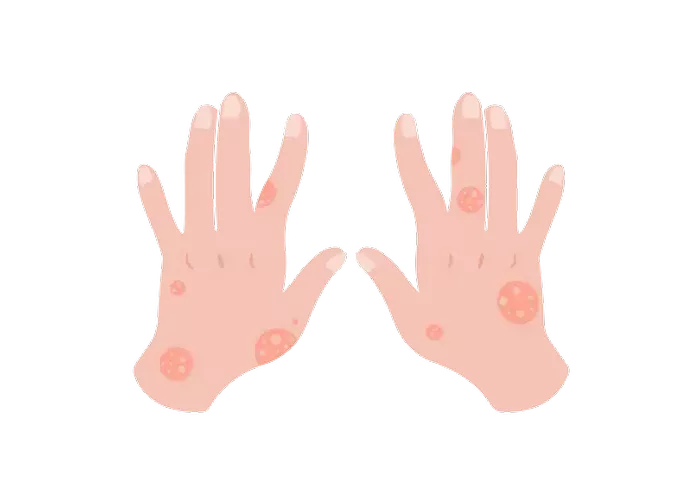
Hidradenitis suppurativa (HS) is a chronic skin condition characterized by painful, inflamed nodules, abscesses, and sinus tracts primarily in areas where skin rubs together, such as the armpits, groin, buttocks, and under the breasts. Despite extensive research, the precise causes of HS remain unclear. However, several contributing factors have been identified, including genetic predisposition, immune system dysfunction, hormonal influences, lifestyle factors, and environmental triggers.
Genetic Predisposition
One of the most significant factors contributing to the development of hidradenitis suppurativa is genetic predisposition. Studies have shown that HS tends to run in families, suggesting a hereditary component. Researchers have identified mutations in genes associated with the condition, particularly those involved in the inflammatory response and skin integrity.
1. Genetic Studies and Family History: Approximately one-third of individuals with HS report a family history of the condition. This familial clustering indicates a genetic link. Specific genetic mutations, such as those in the gamma-secretase complex genes (NCSTN, PSENEN, and PSEN1), have been associated with HS. These genes play a crucial role in the Notch signaling pathway, which is essential for maintaining normal skin cell function and immune response.
2. Mode of Inheritance: HS is believed to follow an autosomal dominant pattern of inheritance with incomplete penetrance. This means that a person only needs one copy of the mutated gene from one parent to inherit the condition, but not everyone who inherits the gene will develop HS.
Immune System Dysfunction
Immune system dysfunction is another critical factor in the pathogenesis of hidradenitis suppurativa. HS is often classified as an autoinflammatory disorder, meaning it involves abnormal activation of the innate immune system.
1. Chronic Inflammation: HS is characterized by chronic inflammation in the hair follicles and surrounding skin. This inflammation is driven by an overactive immune response, leading to the formation of painful nodules and abscesses. Elevated levels of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and interleukin-17 (IL-17), have been found in the affected skin of HS patients.
2. Immune Cell Involvement: Various immune cells, including neutrophils, macrophages, and T cells, are involved in the inflammatory process of HS. Neutrophils, in particular, play a significant role in the formation of abscesses and sinus tracts. Dysregulation of these immune cells contributes to the persistent inflammation seen in HS.
Hormonal Influences
Hormonal factors also play a crucial role in the development and exacerbation of hidradenitis suppurativa. The condition often manifests after puberty and tends to worsen during periods of hormonal fluctuation, such as the menstrual cycle, pregnancy, and menopause.
1. Androgens and Sebaceous Glands: Androgens, which are male hormones present in both men and women, can influence the activity of sebaceous glands and hair follicles. Elevated levels of androgens have been observed in some individuals with HS, leading to increased sebum production and follicular occlusion. This occlusion creates an environment conducive to bacterial overgrowth and inflammation.
2. Hormonal Treatments: Hormonal treatments, such as oral contraceptives and anti-androgen medications like spironolactone, have shown some efficacy in managing HS symptoms. These treatments help regulate hormone levels and reduce the severity of flare-ups, indicating a hormonal link to the condition.
Lifestyle Factors
Several lifestyle factors can contribute to the development and severity of hidradenitis suppurativa. While these factors may not directly cause the condition, they can exacerbate symptoms and trigger flare-ups.
1. Obesity: Obesity is a well-known risk factor for HS. Excess body weight leads to increased friction and pressure on the skin, particularly in areas prone to HS, such as the armpits and groin. The mechanical stress from skin-to-skin contact can promote follicular occlusion and inflammation.
2. Smoking: Smoking is strongly associated with HS and is considered a significant risk factor. The exact mechanisms linking smoking to HS are not fully understood, but it is believed that smoking exacerbates inflammation and impairs the skin’s ability to heal. Smokers with HS often experience more severe symptoms and poorer treatment outcomes.
3. Diet: Although the role of diet in HS is still under investigation, some studies suggest that certain dietary factors may influence the condition. For example, a diet high in dairy products and foods with a high glycemic index may worsen HS symptoms. Conversely, some patients report improvement with dietary modifications, such as reducing dairy intake and adopting an anti-inflammatory diet.
SEE ALSO: What Makes Hidradenitis Suppurativa Worse
Environmental Triggers
Environmental factors can also play a role in triggering or exacerbating hidradenitis suppurativa. These triggers vary from person to person and can include:
1. Heat and Humidity: Hot and humid weather can increase sweating and friction, leading to flare-ups in HS-prone areas. Keeping the affected areas cool and dry can help reduce the risk of exacerbations.
2. Friction and Pressure: Activities that involve prolonged friction or pressure on the skin, such as tight clothing, excessive sweating, or repetitive movements, can trigger HS symptoms. Wearing loose-fitting clothing and using moisture-wicking fabrics can help minimize irritation.
3. Stress: Psychological stress is known to exacerbate many chronic inflammatory conditions, including HS. Stress can trigger the release of stress hormones, such as cortisol, which can worsen inflammation and contribute to flare-ups. Stress management techniques, such as mindfulness, meditation, and counseling, can be beneficial for individuals with HS.
Microbial Factors
The role of microbial factors, including bacteria, in the pathogenesis of hidradenitis suppurativa is an area of ongoing research. While HS is not primarily considered an infectious disease, microbial involvement in the condition’s progression is evident.
1. Bacterial Colonization: The hair follicles and skin of individuals with HS are often colonized by various bacteria, including Staphylococcus aureus and Streptococcus species. These bacteria can contribute to the formation of abscesses and sinus tracts. However, it remains unclear whether bacterial colonization is a primary cause or a secondary effect of the inflammatory process in HS.
2. Biofilms: Biofilms, which are communities of bacteria encased in a protective matrix, have been detected in the skin of HS patients. Biofilms can contribute to chronic inflammation and resistance to antibiotic treatment. Targeting biofilms is an area of interest in developing new treatment strategies for HS.
Conclusion
Hidradenitis suppurativa is a complex and multifactorial condition with no single cause. Instead, it results from the interplay of genetic predisposition, immune system dysfunction, hormonal influences, lifestyle factors, environmental triggers, and microbial involvement. Understanding these contributing factors is essential for developing effective treatments and management strategies for HS.
While there is currently no cure for HS, advances in research are leading to a better understanding of the condition and the development of targeted therapies. Early diagnosis and a comprehensive treatment approach, including medical, surgical, and lifestyle interventions, can help manage symptoms, reduce flare-ups, and improve the quality of life for individuals living with hidradenitis suppurativa.
Related Topics: