Psoriatic arthritis (PsA) is a chronic inflammatory arthritis that affects some people with psoriasis, a skin condition characterized by red, scaly patches that may itch or burn. While PsA primarily affects the joints, causing pain, stiffness, and swelling, many individuals wonder whether the disease can spread to other parts of the body or worsen over time. Understanding the spread and progression of PsA involves exploring its underlying mechanisms, risk factors, and management strategies.
Understanding Psoriatic Arthritis
Psoriatic arthritis is classified as an autoimmune disorder, where the immune system mistakenly attacks healthy tissues, primarily in the joints and skin. The exact cause of PsA is not fully understood, but it is believed to result from a combination of genetic predisposition and environmental triggers.
1. Genetic Factors: Family history plays a significant role in the development of psoriatic arthritis. Individuals with a family member affected by PsA or psoriasis have an increased risk of developing the condition themselves. Specific genetic markers, such as variations in certain human leukocyte antigen (HLA) genes, have been linked to susceptibility to PsA.
2. Immune System Dysfunction: PsA is characterized by chronic inflammation, which leads to joint damage and other symptoms. Immune cells, particularly T cells and cytokines (such as tumor necrosis factor-alpha or TNF-α), play a crucial role in the inflammatory processes seen in PsA.
3. Psoriasis and Joint Involvement: Many individuals with PsA have psoriasis, but not all people with psoriasis develop PsA. Psoriasis usually precedes the onset of PsA, often by several years. The severity of psoriasis does not necessarily correlate with the severity of PsA.
Does Psoriatic Arthritis Spread?
One of the common concerns among individuals diagnosed with PsA is whether the disease can spread beyond the joints or if it can worsen over time. Here’s a detailed exploration of the spread and progression of PsA:
Joint Progression and Damage
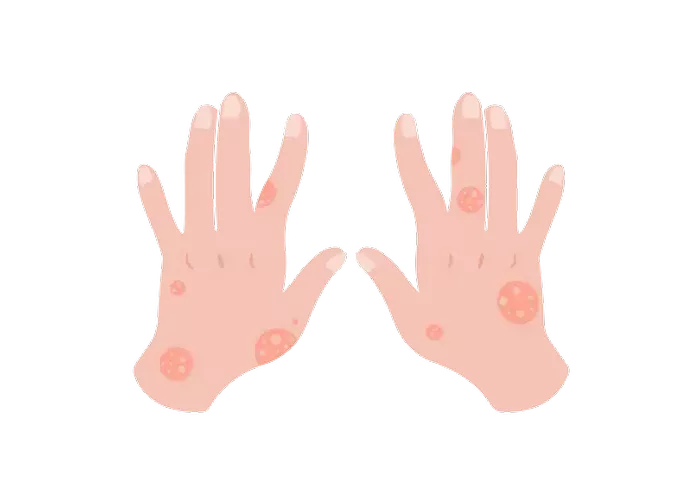
Psoriatic arthritis primarily affects the joints, causing inflammation that can lead to pain, stiffness, swelling, and eventually joint damage if left untreated. The disease can affect any joint in the body, including the fingers, toes, wrists, knees, ankles, and spine.
1. Progression of Joint Symptoms: PsA is known for its variable course and unpredictable progression. Some individuals may experience mild, intermittent symptoms that do not worsen significantly over time, while others may develop more severe joint involvement and progressive damage.
2. Joint Damage and Disability: Without proper management, chronic inflammation in PsA can lead to irreversible joint damage, deformities, and disability. Early diagnosis and aggressive treatment are crucial for preventing or minimizing joint damage and preserving joint function.
Extra-Articular Manifestations
While PsA primarily affects the joints, it can also involve other parts of the body, leading to various extra-articular manifestations:
1. Skin Involvement: Many individuals with PsA also have psoriasis, which involves the skin. Psoriasis symptoms may worsen concurrently with joint symptoms, but the severity of skin involvement does not necessarily correlate with the severity of joint disease.
2. Nail Changes: Nail psoriasis is common in individuals with PsA and can cause changes such as pitting, thickening, discoloration, and separation of the nail from the nail bed (onycholysis).
3. Enthesitis: Enthesitis is inflammation at the site where tendons or ligaments insert into the bone. It commonly affects the Achilles tendon and the plantar fascia in the feet, causing pain, swelling, and stiffness.
4. Dactylitis: Dactylitis, also known as “sausage digit,” is swelling of an entire finger or toe. It is a hallmark feature of PsA and can be very painful and disabling.
5. Eye Involvement: Some individuals with PsA may develop inflammation in the eyes, known as uveitis or iritis. Eye inflammation requires prompt medical attention to prevent complications and preserve vision.
SEE ALSO: Optimal Infusion Therapies for Managing Psoriatic Arthritis
Progression Over Time
The progression of PsA varies widely among individuals and can be influenced by several factors:
1. Severity of Inflammation: The intensity and duration of inflammation play a crucial role in the progression of PsA. Persistent inflammation can lead to progressive joint damage and worsening symptoms.
2. Treatment Response: Early initiation of effective treatment is associated with better outcomes and reduced progression of PsA. Treatments aim to control inflammation, manage symptoms, and prevent joint damage.
3. Risk Factors: Certain factors may increase the risk of disease progression in PsA, including older age at diagnosis, presence of erosive disease (joint damage visible on X-ray), high disease activity, and presence of certain autoantibodies.
Management Strategies
Managing PsA involves a multidisciplinary approach aimed at controlling symptoms, preventing joint damage, and improving quality of life:
1. Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), biologic therapies (such as TNF inhibitors), and targeted synthetic DMARDs are commonly used to reduce inflammation and slow disease progression.
2. Physical Therapy: Physical therapy and exercise programs can help improve joint mobility, strengthen muscles, and reduce pain and stiffness.
3. Lifestyle Modifications: Maintaining a healthy weight, avoiding smoking, managing stress, and protecting joints from excessive strain can help manage symptoms and improve overall well-being.
4. Regular Monitoring: Regular follow-up with healthcare providers is essential to monitor disease activity, adjust treatment as needed, and address any new symptoms or complications.
Conclusion
Psoriatic arthritis is a chronic condition characterized by inflammation of the joints and, in some cases, involvement of other organs and tissues. While PsA primarily affects the joints, leading to pain, stiffness, and potential joint damage, it can also involve the skin, nails, eyes, and other areas of the body. The progression of PsA varies among individuals, influenced by genetic factors, immune system dysfunction, treatment efficacy, and lifestyle factors.
While PsA is not considered to “spread” in the traditional sense to unaffected joints or organs, it can progress in terms of joint damage and the involvement of additional body systems over time. Early diagnosis, comprehensive management, and adherence to treatment recommendations are essential for optimizing outcomes and improving quality of life for individuals living with psoriatic arthritis. Ongoing research continues to enhance our understanding of PsA and develop new therapies aimed at controlling disease progression and improving long-term outcomes.
Related Topics: