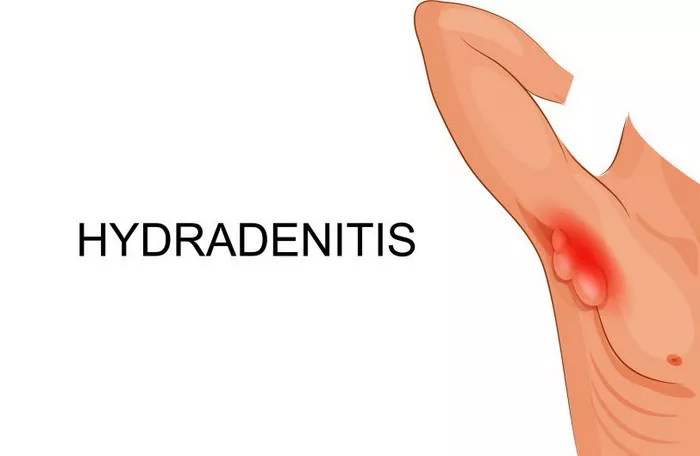
Hidradenitis suppurativa (HS) is a chronic, inflammatory skin condition characterized by painful nodules, abscesses, and sinus tracts typically occurring in areas where skin rubs together, such as the armpits, groin, and buttocks. This debilitating disease impacts a significant number of individuals worldwide, with varying degrees of severity and symptomatology. A critical question that arises among patients and healthcare professionals alike is whether HS could increase the risk of developing cancer. This article delves into the relationship between hidradenitis suppurativa and cancer, exploring current research, understanding the potential mechanisms, and analyzing the implications for patients.
Understanding Hidradenitis Suppurativa
Hidradenitis suppurativa is marked by recurring, painful nodules and abscesses, primarily in apocrine gland-bearing areas. The pathogenesis of HS remains incompletely understood, but it is believed to involve follicular occlusion, dysregulated immune response, and genetic predisposition. The condition typically progresses through stages, from mild manifestations of tender nodules to more severe forms with extensive scarring and sinus tract formation.
The Connection Between Chronic Inflammation and Cancer
The association between chronic inflammation and cancer is well-documented in medical literature. Chronic inflammation is a persistent inflammatory response that can lead to cellular damage, genetic mutations, and an environment conducive to cancer development. HS, with its recurrent inflammatory processes, raises concerns about a potential link to cancer. Chronic inflammation in HS may involve the release of pro-inflammatory cytokines, oxidative stress, and tissue remodeling, all of which can influence carcinogenesis.
Review of Research on HS and Cancer Risk
A variety of studies have investigated the potential association between hidradenitis suppurativa and different types of cancer. This section reviews significant findings and the implications of these studies for understanding the cancer risk in individuals with HS.
1. Skin Cancer
Several studies have explored the potential link between HS and skin cancer, particularly squamous cell carcinoma (SCC) and basal cell carcinoma (BCC). Chronic skin inflammation and repeated trauma from HS lesions could theoretically increase the risk of skin cancer. Research findings, however, are mixed. While some studies suggest a higher incidence of skin cancer among HS patients, others have not demonstrated a statistically significant association. For instance, a retrospective study published in The Journal of Dermatology found an increased incidence of SCC in patients with severe HS, though the overall risk was still considered relatively low.
2. Breast Cancer
Breast cancer is another area of concern due to the common anatomical locations affected by HS. A study published in Breast Cancer Research and Treatment examined the cancer risk in women with HS and found a modest increase in breast cancer risk. The researchers hypothesized that chronic inflammation and hormonal changes associated with HS could contribute to this risk. However, more extensive studies are required to establish a definitive relationship and understand the underlying mechanisms.
3. Other Cancers
Research on the association between HS and other types of cancer, such as colorectal cancer or lymphoma, is limited. Some studies have suggested a possible increased risk of lymphoma in patients with severe HS, but the evidence remains inconclusive. The association with colorectal cancer has not been well-established, and further investigation is needed to determine if HS contributes to an elevated risk for these cancers.
Mechanisms Linking HS to Cancer Risk
To better understand the potential link between HS and cancer, it’s essential to explore the mechanisms through which chronic inflammation and HS might contribute to carcinogenesis.
1. Chronic Inflammation
Chronic inflammation is a well-known risk factor for cancer. In HS, the persistent inflammatory response can lead to repeated cycles of tissue damage and repair, potentially resulting in genetic mutations and an increased risk of cancer. The release of pro-inflammatory cytokines and reactive oxygen species during inflammation can also contribute to DNA damage and promote carcinogenic processes.
SEE ALSO: Does Ice Help Hidradenitis Suppurativa?
2. Altered Immune Response
HS is characterized by an abnormal immune response, which may play a role in increasing cancer risk. Dysregulation of the immune system can lead to an environment that supports tumor growth and progression. Additionally, immunosuppressive therapies used to manage severe HS could potentially impact cancer risk, although this connection is still under investigation.
3. Genetic Predisposition
Genetic factors may influence both HS and cancer susceptibility. Certain genetic mutations or polymorphisms may predispose individuals to both chronic inflammatory conditions and cancer. Identifying common genetic pathways could help clarify the relationship between HS and cancer risk.
Clinical Implications for HS Patients
For patients with hidradenitis suppurativa, understanding the potential cancer risk is crucial for informed decision-making and effective management. Here are some key clinical implications:
1. Regular Surveillance
Patients with severe HS should undergo regular dermatological evaluations to monitor for potential skin cancers, particularly if they have a history of recurrent lesions or significant scarring. Early detection and intervention are critical for managing skin cancer and improving outcomes.
2. Awareness and Education
Healthcare providers should educate HS patients about the potential risks and symptoms of associated cancers. Awareness can lead to earlier detection and more effective management of potential malignancies.
3. Multidisciplinary Approach
A multidisciplinary approach involving dermatologists, oncologists, and other specialists may be beneficial for managing HS and addressing any potential cancer risks. Collaboration among healthcare providers can ensure comprehensive care and optimize patient outcomes.
Future Research Directions
To better understand the relationship between hidradenitis suppurativa and cancer, future research should focus on the following areas:
1. Large-Scale Epidemiological Studies
Conducting large-scale epidemiological studies can help clarify the association between HS and various types of cancer. These studies should include diverse populations and consider factors such as disease severity, treatment modalities, and genetic predisposition.
2. Mechanistic Studies
Investigating the underlying mechanisms linking chronic inflammation in HS to cancer development can provide valuable insights. Research into the role of specific cytokines, immune cells, and genetic factors could elucidate the pathways involved.
3. Clinical Trials
Clinical trials exploring the impact of different treatment strategies on cancer risk in HS patients are needed. Evaluating the safety and efficacy of various therapies can help determine their potential influence on cancer risk and guide clinical decision-making.
Conclusion
Hidradenitis suppurativa, with its chronic inflammatory nature, raises valid concerns about an increased risk of cancer. While current research indicates a potential association between HS and certain cancers, the evidence is not yet definitive. Understanding the mechanisms linking HS to cancer, coupled with regular surveillance and a multidisciplinary approach, can help manage potential risks and improve patient outcomes. Ongoing research will be crucial in providing more conclusive evidence and enhancing our understanding of the relationship between HS and cancer.
Related Topics: