Dyshidrosis, also known as dyshidrotic eczema or pompholyx, is a skin condition characterized by small, itchy blisters that usually appear on the hands and feet. These blisters can be extremely uncomfortable, leading to itching, burning sensations, and sometimes pain. Despite the name, dyshidrosis is not directly caused by sweat glands. In this article, we’ll explore the causes, triggers, and factors associated with dyshidrosis in detail.
Understanding Dyshidrosis
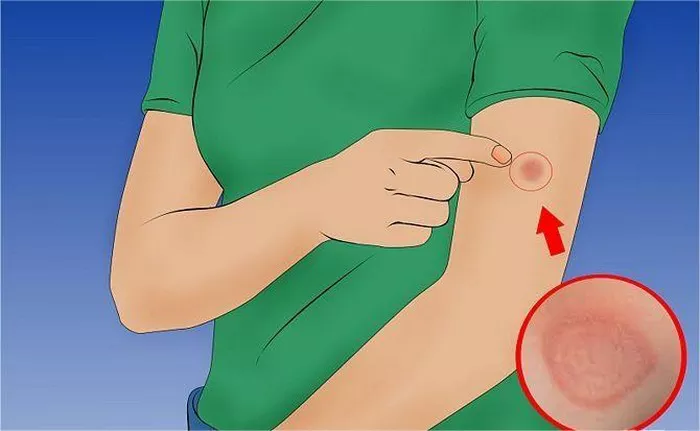
Dyshidrosis manifests as tiny blisters filled with fluid, often occurring on the sides of the fingers, palms of the hands, or soles of the feet. The blisters tend to cluster together and can last for about two to four weeks. They may dry out, peel, or become flaky, leaving the skin dry and cracked. Although it is not contagious, dyshidrosis can be a recurring condition, and its flare-ups are often unpredictable.
Who Is Affected by Dyshidrosis?
Dyshidrosis can affect anyone, but it is most common in adults between the ages of 20 and 40. It tends to occur more frequently in women than men. The condition is also more common in people who have a history of other skin conditions, such as atopic dermatitis or other types of eczema. Those who work in professions requiring frequent hand washing, use of chemicals, or prolonged contact with water (such as healthcare workers, cleaners, or hairdressers) may be at higher risk.
What Are the Causes of Dyshidrosis?
The exact cause of dyshidrosis is not fully understood. However, several factors are known to contribute to its development and flare-ups. Dyshidrosis is often linked to underlying conditions, allergies, or external factors. Below are the most recognized causes:
1. Allergies and Sensitivities
One of the most common triggers for dyshidrosis is an allergic reaction. People who suffer from hay fever, asthma, or contact dermatitis are more likely to experience dyshidrosis. Allergens such as certain metals, fragrances, or chemicals can cause flare-ups.
Nickel Allergy: A significant number of people with dyshidrosis have a sensitivity to nickel, a metal commonly found in everyday items like jewelry, watches, and even certain foods. Nickel exposure can lead to an allergic reaction, which may trigger the blisters associated with dyshidrosis.
Cobalt Sensitivity: Cobalt, another metal, can also cause allergic reactions in some people. It is often found in items like paints, certain medical implants, and vitamin supplements. When people who are sensitive to cobalt are exposed to this metal, it may cause their dyshidrosis to flare up.
Fragrances and Chemicals: Many skin-care products contain fragrances or chemicals that can irritate sensitive skin. Those with dyshidrosis should be cautious when using soaps, lotions, or detergents, as some ingredients may provoke a reaction.
SEE ALSO: What is in Aveeno Eczema Cream?
2. Stress
Stress is another well-known trigger for dyshidrosis. Emotional and physical stress can impact the body’s immune system, which may lead to skin flare-ups. When the body is under stress, it releases hormones like cortisol that can weaken the skin barrier, making the skin more prone to inflammation and blisters.
Emotional Stress: Anxiety, depression, and general emotional tension have all been linked to worsening dyshidrosis. Stress can also lead to behaviors that aggravate the condition, such as excessive scratching.
Physical Stress: Physical exertion, illness, or fatigue can strain the body, leading to immune system dysregulation, which may trigger dyshidrosis.
3. Sweating and Moisture
Although dyshidrosis is not directly caused by sweat glands, excessive sweating and moisture can contribute to flare-ups. People with hyperhidrosis (excessive sweating) are at a higher risk of developing dyshidrosis, as sweat can create an environment that irritates the skin.
Hot and Humid Weather: Dyshidrosis is often worse during the warmer months when the skin is exposed to heat and humidity. Sweat can accumulate on the hands and feet, causing irritation and increasing the likelihood of blisters.
Prolonged Moisture Exposure: Keeping hands or feet in water for extended periods or wearing gloves or shoes that trap moisture can trigger dyshidrosis. This is why professions requiring frequent hand washing or the use of gloves are linked to higher rates of the condition.
4. Fungal Infections
Fungal infections, especially those affecting the feet (such as athlete’s foot), have been associated with dyshidrosis. It is believed that the presence of a fungal infection can cause an immune response that leads to the formation of blisters.
Tinea Pedis: A common fungal infection of the feet, tinea pedis, may coexist with dyshidrosis. Treating the fungal infection can sometimes alleviate the symptoms of dyshidrosis.
5. Atopic Dermatitis
Atopic dermatitis, a chronic form of eczema, is often seen in people with dyshidrosis. The two conditions share some similarities, such as itchy, inflamed skin, and a weakened skin barrier. People who have a history of atopic dermatitis are more prone to developing dyshidrosis, particularly during flare-ups of their underlying eczema.
Other Contributing Factors
Besides the main causes mentioned above, several other factors may contribute to dyshidrosis flare-ups.
1. Genetic Predisposition
There is evidence to suggest that genetics play a role in the development of dyshidrosis. If a family member has a history of eczema, allergies, or asthma, there is an increased likelihood of developing dyshidrosis. This genetic link indicates that the condition may be inherited, although more research is needed to fully understand the connection.
2. Immune System Dysfunction
Dyshidrosis is believed to involve the immune system. It may be triggered by immune system overactivity, similar to other eczema-related conditions. People with autoimmune diseases or weakened immune systems are more susceptible to developing dyshidrosis.
3. Environmental Factors
The environment can also play a role in dyshidrosis flare-ups. Factors such as air pollution, allergens in the home (dust mites, pet dander), and irritants in the workplace can worsen symptoms.
4. Medications
Certain medications may trigger dyshidrosis in some individuals. For example, medications that affect the immune system, such as immunosuppressants, or treatments for other skin conditions, may have side effects that contribute to the development of dyshidrosis.
5. Smoking
There is some evidence to suggest that smoking may be a risk factor for developing dyshidrosis. The chemicals in tobacco smoke can irritate the skin and weaken the immune system, potentially triggering a flare-up.
Diagnosing Dyshidrosis
A healthcare provider can diagnose dyshidrosis based on the appearance of the blisters and the patient’s medical history. In some cases, patch testing may be used to determine if an allergic reaction to a specific substance is triggering the condition. If a fungal infection is suspected, a skin scraping may be taken to rule out other causes of the blisters.
Managing and Treating Dyshidrosis
Although there is no cure for dyshidrosis, the condition can be managed with appropriate treatment and lifestyle changes. Treatment typically focuses on relieving symptoms, preventing infections, and reducing the likelihood of future flare-ups.
1. Topical Steroids
One of the most common treatments for dyshidrosis is the application of topical corticosteroids. These medications can help reduce inflammation and relieve itching. In severe cases, a healthcare provider may prescribe stronger steroid creams or ointments.
2. Moisturizers and Barrier Creams
Keeping the skin well-moisturized is crucial in managing dyshidrosis. Using heavy-duty moisturizers or barrier creams can help repair the skin’s protective barrier and prevent blisters from forming.
3. Antihistamines
If an allergic reaction is suspected, antihistamines may be used to control itching and reduce the body’s histamine response, which can trigger flare-ups.
4. Avoiding Triggers
Identifying and avoiding triggers is one of the most effective ways to manage dyshidrosis. This may involve avoiding exposure to allergens, such as nickel or cobalt, using fragrance-free skin-care products, and reducing stress.
5. Cold Compresses
Applying cold compresses to affected areas can provide temporary relief from itching and reduce the severity of the blisters.
6. Phototherapy
In severe cases, phototherapy (light therapy) may be used to treat dyshidrosis. This treatment involves exposing the skin to controlled amounts of ultraviolet light, which can reduce inflammation and improve symptoms.
Conclusion
Dyshidrosis is a complex skin condition with multiple causes and triggers. While its exact cause remains unclear, factors such as allergies, stress, moisture, and underlying skin conditions all play a significant role in its development. Although there is no cure, understanding what causes dyshidrosis and how to manage it can help prevent flare-ups and improve quality of life. Working with a healthcare provider to identify triggers and develop an appropriate treatment plan is essential for managing this condition.