Hidradenitis suppurativa (HS) is a chronic skin condition that affects hair follicles and sweat glands. It is often painful and causes recurring lumps, abscesses, and tunnels under the skin. While the exact cause of HS is not entirely understood, it is considered to have an autoimmune component. In this article, we will explore what HS is, its autoimmune nature, how it develops, and what treatments are available.
Understanding Hidradenitis Suppurativa
Hidradenitis suppurativa (HS) is a long-term skin condition that primarily affects areas of the body where skin rubs together, such as the armpits, groin, buttocks, and under the breasts. It usually starts as small, painful lumps under the skin. These lumps can become infected, leading to abscesses and tunnels, also known as fistulas. These symptoms often worsen over time.
HS is not an infection, and it is not caused by poor hygiene, though it can become complicated by bacterial infections due to the skin’s open wounds.
Is Hidradenitis Suppurativa an Autoimmune Disease?
HS is considered to have autoimmune characteristics because the immune system seems to play a role in its development. In an autoimmune disease, the body’s immune system mistakenly attacks healthy tissue. In the case of HS, the immune system overreacts to hair follicles that become clogged or irritated, triggering inflammation and causing lesions in the skin.
While it is not strictly classified as an autoimmune disorder like lupus or rheumatoid arthritis, research has suggested that immune system dysregulation is involved. HS is classified as an inflammatory skin disease, with autoimmune factors contributing to its progression.
SEE ALSO: How Do I Know If I Have Hidradenitis Suppurativa (HS)?
What Causes Hidradenitis Suppurativa?
The exact cause of HS is not well understood, but several factors contribute to the condition:
Clogged Hair Follicles: HS starts when hair follicles become blocked. This may be due to sweat, oil, or other debris.
Immune System Response: When hair follicles clog, the immune system reacts, causing inflammation in the surrounding skin tissue. This can lead to the formation of abscesses, nodules, and tunnels.
Genetic Factors: Many people with HS have a family history of the condition. It is believed that genetic mutations affecting the immune system may make some people more prone to developing HS.
Hormonal Influence: Hormones are also thought to play a role, as HS often starts after puberty and can worsen during menstruation, pregnancy, or hormonal changes.
Symptoms of Hidradenitis Suppurativa
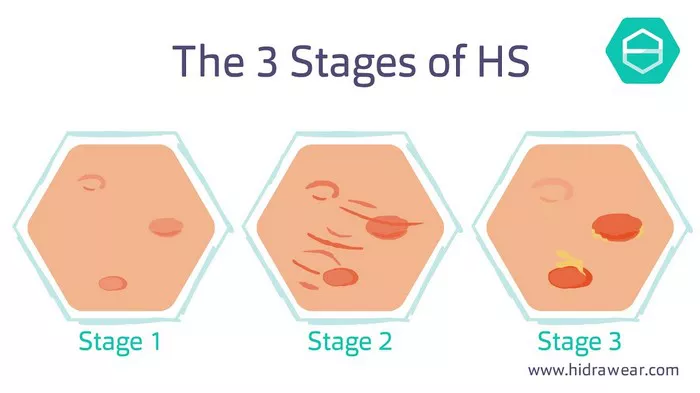
HS has several stages of severity, known as Hurley stages, and symptoms can range from mild to severe. The symptoms include:
Painful Bumps: The first sign of HS is often small, painful lumps or boils under the skin, commonly found in the armpits, groin, and other areas with skin-to-skin contact.
Recurring Abscesses: These bumps can grow into larger, painful abscesses filled with pus. The abscesses may burst and drain fluid, which can lead to infection.
Tunnels and Scars: Over time, tunnels (fistulas) can form under the skin, connecting abscesses. This can cause scarring and permanent damage to the affected areas.
Foul Odor: The drainage from abscesses can produce a foul smell, which can be distressing for individuals living with HS.
The Autoimmune Connection in HS
Though the immune system is designed to protect the body from harmful bacteria and viruses, in people with HS, the immune system mistakenly targets the skin’s hair follicles. This misguided immune response leads to inflammation, pain, and abscesses.
In autoimmune conditions, the immune system becomes hyperactive, producing inflammation even when there is no actual threat, such as bacteria or an infection. In HS, this inflammatory response is directed at the hair follicles and surrounding tissues. Researchers believe that genetic predispositions, environmental factors, and hormonal changes can trigger the immune system to react abnormally in people with HS.
Is HS Related to Other Autoimmune Diseases?
People with HS are more likely to have other autoimmune or inflammatory conditions, such as:
Crohn’s Disease: An inflammatory bowel disease that affects the digestive tract.
Psoriasis: A skin condition that causes red, scaly patches on the skin.
Rheumatoid Arthritis: An autoimmune disease that causes joint inflammation.
These associations further support the idea that HS may involve an abnormal immune system response.
Diagnosis of Hidradenitis Suppurativa
Diagnosing HS can be challenging because its symptoms often resemble other skin conditions such as boils or cysts. However, dermatologists diagnose HS based on:
Physical Examination: A doctor will examine the affected areas of the skin, looking for typical HS symptoms like recurring lumps, abscesses, and tunnels.
Medical History: The doctor will ask about the frequency and severity of flare-ups, as well as any family history of skin conditions or autoimmune diseases.
Imaging: In some cases, an ultrasound or MRI might be used to look at the tunnels under the skin.
Treatment for Hidradenitis Suppurativa
While there is no cure for HS, several treatments can help manage symptoms and prevent flare-ups.
1. Topical Treatments
Topical treatments include creams or ointments applied directly to the skin to reduce inflammation and infection. Common topical treatments for HS include:
Antibiotic Creams: These can help prevent or control infection in abscesses.
Corticosteroids: These reduce inflammation and can help control flare-ups.
2. Oral Medications
For moderate to severe HS, oral medications may be prescribed. These include:
Antibiotics: Oral antibiotics can help control bacterial infections and reduce inflammation.
Hormonal Therapy: Hormone-regulating medications, such as birth control pills, can help women whose HS flares up during menstruation.
Immunosuppressants: These medications, like biologics, reduce the activity of the immune system and help manage inflammation. Biologics, such as adalimumab (Humira), target specific parts of the immune system involved in HS.
Retinoids: These medications are derived from vitamin A and help reduce the production of oil and dead skin that clogs follicles.
3. Surgical Treatment
In severe cases, surgery may be needed to remove abscesses, tunnels, or scar tissue.
Incision and Drainage: This involves draining large abscesses to relieve pain and pressure. However, the condition may recur in the same area.
Laser Surgery: Laser treatments can help remove affected skin and hair follicles to reduce the likelihood of new lesions.
Excision Surgery: In severe cases, the affected area may need to be surgically removed. This is a more invasive procedure and is used when other treatments are ineffective.
Lifestyle Changes for Managing HS
Certain lifestyle changes can help people with HS manage their condition and reduce flare-ups:
Weight Management: Maintaining a healthy weight can reduce friction between skin folds, which may help prevent flare-ups in areas like the armpits and groin.
Avoid Tight Clothing: Wearing loose, breathable clothing can minimize irritation and allow air circulation to reduce sweating.
Smoking Cessation: Smoking has been linked to increased HS severity. Quitting smoking may help reduce symptoms.
Healthy Diet: Some studies suggest that avoiding foods that trigger inflammation, such as dairy and high-sugar foods, can help manage HS.
Living with Hidradenitis Suppurativa
HS is a challenging condition that can affect quality of life due to its painful and recurring symptoms. However, with proper management, many people can reduce the frequency and severity of flare-ups. The key is working closely with healthcare providers to develop a personalized treatment plan that includes medications, lifestyle changes, and possibly surgery.
Support groups and counseling may also be helpful for individuals dealing with the emotional and psychological impact of HS. It is essential to address not only the physical symptoms but also the mental and emotional well-being of people living with this chronic condition.
Conclusion
Hidradenitis suppurativa is a complex and often painful autoimmune-related condition. It primarily affects areas of the body where skin rubs together, causing abscesses, tunnels, and scarring. While the cause of HS is not fully understood, it is believed to involve an abnormal immune response to clogged hair follicles.
Though there is no cure for HS, various treatments, including topical and oral medications, lifestyle changes, and surgery, can help manage symptoms. If you suspect you have HS, consult with a healthcare provider to get an accurate diagnosis and develop a treatment plan tailored to your needs.