Hidradenitis Suppurativa (HS) is a chronic skin condition that causes painful bumps and abscesses, primarily in areas where skin rubs together, such as the armpits, groin, and under the breasts. Many people wonder if HS is an autoimmune disease. In this article, we will explore the nature of HS, its causes, symptoms, and the ongoing debate regarding its classification.
Understanding Hidradenitis Suppurativa
What is Hidradenitis Suppurativa?
Hidradenitis Suppurativa is characterized by inflamed skin lesions that can lead to scarring and discomfort. The condition usually begins after puberty and can persist throughout a person’s life. Lesions can become painful and may drain pus. This can significantly affect a person’s quality of life.
Symptoms of Hidradenitis Suppurativa
The symptoms of HS include:
Painful Bumps: These can be pea-sized or larger and often appear in clusters.
Abscesses: The bumps can turn into abscesses that may burst and drain fluid.
Scarring: Recurrent lesions can lead to thickened skin and scarring.
Foul Odor: Infected lesions may produce a strong, unpleasant smell.
Itching and Burning: Many individuals report discomfort in affected areas.
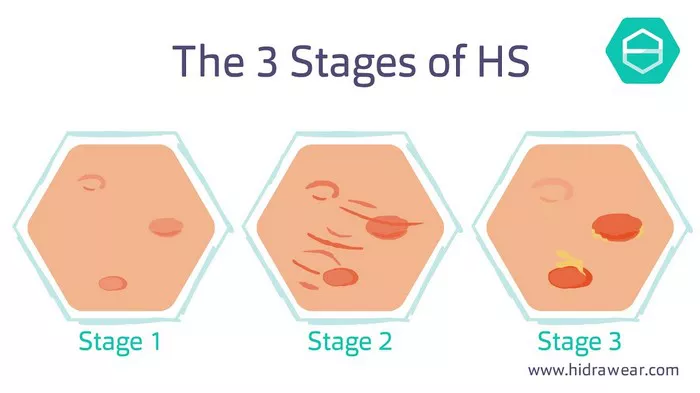
Stages of Hidradenitis Suppurativa
HS is often classified into three stages:
Stage 1 (Mild): Involves single or multiple abscesses without scarring.
Stage 2 (Moderate): Characterized by recurrent abscesses and some scarring.
Stage 3 (Severe): Involves widespread lesions, significant scarring, and sinus tract formation.
Is Hidradenitis Suppurativa Autoimmune?
Defining Autoimmune Diseases
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own tissues. This can result in inflammation and damage to various organs and systems. Common autoimmune diseases include rheumatoid arthritis, lupus, and multiple sclerosis.
The Debate Surrounding HS
Researchers and dermatologists have debated whether HS should be classified as an autoimmune disease. Here are some key points in this discussion:
Inflammation in HS
While HS does involve inflammation, similar to autoimmune diseases, this alone does not mean it is autoimmune. In HS, inflammation is triggered by various factors, including:
- Blocked Hair Follicles: The condition often starts with clogged hair follicles.
- Bacterial Infections: Secondary infections can exacerbate inflammation.
- Genetic Factors: A family history of HS may increase risk.
Immune System Response
In HS, the immune response is more complex than in traditional autoimmune diseases. Some studies suggest that HS may involve dysregulation of the immune system rather than a straightforward autoimmune process.
Association with Other Conditions
HS is often associated with other inflammatory conditions, such as Crohn’s disease and metabolic syndrome. This association further complicates the classification of HS as autoimmune.
Current Understanding of HS
Risk Factors for Hidradenitis Suppurativa
Several factors may increase the likelihood of developing HS:
Genetics: A family history of HS may predispose individuals to the condition.
Obesity: Excess weight can contribute to friction in skin folds.
Smoking: Tobacco use has been linked to HS severity.
Hormones: Hormonal changes can trigger flare-ups.
Diagnosis of Hidradenitis Suppurativa
Diagnosing HS typically involves:
Medical History: Doctors will ask about symptoms and family history.
Physical Examination: A thorough examination of the affected areas.
Biopsy: In some cases, a small skin sample may be taken to rule out other conditions.
Treatment Options for Hidradenitis Suppurativa
While there is no cure for HS, several treatment options can help manage symptoms:
Topical Treatments
- Antibiotics: Topical antibiotics can reduce bacteria and inflammation.
- Retinoids: These can help unclog pores and reduce lesions.
Oral Medications
- Antibiotics: Oral antibiotics may be prescribed for severe cases.
- Hormonal Therapy: Hormonal treatments can help some patients, especially women.
Surgical Options
- Incision and Drainage: This can relieve pain from abscesses.
- Surgical Removal: In severe cases, removing affected skin may be necessary.
Biologic Treatments
Newer treatments, called biologics, target specific pathways in the immune system. These are often used for severe HS that has not responded to other treatments.
Living with Hidradenitis Suppurativa
Coping Strategies
Living with HS can be challenging. Here are some tips to manage the condition:
Maintain Hygiene: Keep affected areas clean and dry to prevent infections.
Wear Loose Clothing: This can reduce friction and irritation.
Healthy Diet: A balanced diet may help improve overall health and manage weight.
Support Groups: Connecting with others who have HS can provide emotional support.
Mental Health Considerations
The physical symptoms of HS can lead to emotional distress. It is important to address mental health and seek support if needed. Therapy and counseling can be beneficial for those struggling with the psychological impact of HS.
Conclusion
In summary, the classification of Hidradenitis Suppurativa as an autoimmune disease is still a topic of debate. While it shares some characteristics with autoimmune conditions, HS is likely best described as a chronic inflammatory skin condition influenced by various factors, including genetics and the immune response. Understanding HS can help individuals seek appropriate treatment and manage their symptoms effectively. If you suspect you have HS or are experiencing symptoms, consult a healthcare professional for a proper diagnosis and treatment plan.
This comprehensive understanding can empower individuals to cope with HS, seek treatment options, and improve their quality of life.
Related topics: