The Course of Shingles Infection
Prodromal Phase: Before the characteristic rash appears, patients often experience a prodromal phase. This can last for about 1 – 3 days and may include symptoms such as mild pain, itching, or tingling in a specific area of the body. During this stage, the virus is present in the body, but the risk of transmission is relatively low as there are no visible signs of the infection that can easily spread the virus. For example, a patient may feel a dull ache in one side of the torso and have a mild sense of discomfort, but without any blisters or skin lesions that could release the virus.
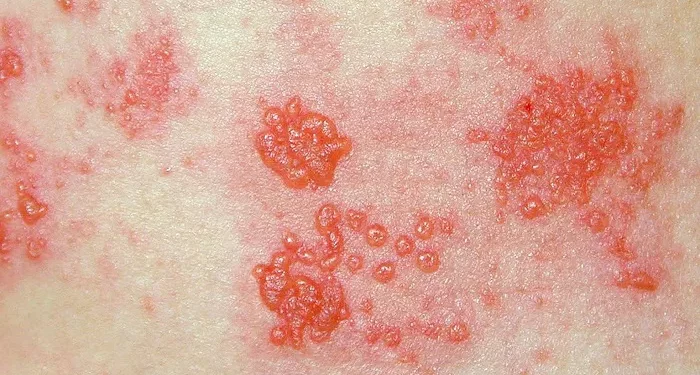
Rash Onset and Development: Once the rash appears, which typically occurs within 2 – 5 days after the start of the prodromal symptoms, the contagiousness begins to increase. The rash starts as small red patches that quickly progress to fluid-filled blisters. These blisters are filled with the varicella-zoster virus and are the main source of transmission. As the blisters form and multiply, the risk of spreading the virus to others becomes more significant. For instance, if a person touches the blister fluid and then touches their own mucous membranes, they could potentially become infected.
Contagiousness during Different Stages of the Rash
Blister Formation Stage: When the blisters first form, they are fragile and can easily rupture. This stage usually lasts for about 3 – 7 days. During this period, the virus is highly concentrated in the blister fluid, and direct contact with the fluid is the most likely mode of transmission. A person with shingles in this stage should take extra precautions to avoid contact with others, especially those who have not had chickenpox or are immunocompromised. For example, a patient with shingles on the face should avoid close contact with children who may not have been exposed to the varicella-zoster virus.
Blister Rupture and Crusting Stage: As the blisters rupture, they release the virus, and the fluid dries to form crusts. This stage can last for approximately 3 – 5 days. Although the risk of transmission decreases as the blisters crust over, the virus can still be present in the crusts. Therefore, it is important to continue taking precautions until the crusts have completely fallen off. For instance, a patient should avoid sharing towels or clothing during this time to prevent the spread of any remaining virus.
Factors Affecting the Duration of Contagiousness
Immune System Function: The strength of an individual’s immune system plays a crucial role in determining how long they remain contagious. A person with a healthy immune system is generally able to control the replication of the virus more effectively, which may lead to a shorter contagious period. In contrast, immunocompromised individuals, such as those with HIV/AIDS, undergoing chemotherapy, or who have had an organ transplant, may have a longer duration of contagiousness as their bodies are less able to fight off the virus. For example, a cancer patient receiving chemotherapy may shed the virus for a more extended period compared to a healthy adult with shingles.
Treatment Received: Early initiation of appropriate antiviral treatment can help to reduce the duration of the shingles infection and potentially shorten the contagious period. Antiviral medications work by inhibiting the replication of the varicella-zoster virus. If a patient starts treatment soon after the onset of symptoms, the virus may be cleared from the body more quickly, reducing the time during which they can transmit the virus. For instance, a patient who begins antiviral therapy within 72 hours of the appearance of the rash may have a less severe infection and a shorter contagious phase.
Contagiousness to Different Populations
Individuals without a History of Chickenpox: People who have never had chickenpox are highly susceptible to contracting the varicella-zoster virus from a person with shingles. When exposed, they can develop a primary varicella infection. The contagious period is of particular concern when dealing with such individuals, as they have no pre-existing immunity. For example, in a school or daycare setting, if a staff member has shingles, children who have not had chickenpox are at risk, and precautions need to be taken until the staff member is no longer contagious.
Immunocompromised Individuals: As mentioned earlier, immunocompromised individuals are at increased risk of both contracting shingles and experiencing a more severe form of the infection. They are also more likely to have a prolonged contagious period. Their weakened immune systems make it difficult for them to clear the virus, and they may continue to shed the virus for a longer time. For example, a patient with an autoimmune disorder may require more vigilant isolation measures due to the extended risk of transmission.
Prevention and Precautions during the Contagious Period
Isolation and Quarantine: Isolating the patient with shingles, especially during the peak contagious period when the blisters are present and active, is an important preventive measure. This can involve keeping the patient in a separate room and limiting their contact with others. In a hospital or care facility, strict isolation protocols are often implemented to protect other patients and healthcare workers. For example, a patient with shingles may be placed in a private room with restricted visitation until the risk of transmission is significantly reduced.
Hygiene Practices: Good personal hygiene is essential. The patient should cover the affected area with clean, dry bandages to prevent the spread of blister fluid. Frequent handwashing is also crucial, both for the patient and for those in contact with the patient. Additionally, any objects or surfaces that come into contact with the patient or the blister fluid should be cleaned and disinfected regularly. For instance, bedding, clothing, and utensils used by the patient should be washed separately in hot water and detergent.
Conclusion
In conclusion, the duration of contagiousness in shingles varies depending on several factors. The initial prodromal phase has a relatively low risk of transmission, while the blister formation and rupture stages are the most contagious, lasting approximately 3 – 7 days and 3 – 5 days respectively. However, the overall contagious period can be influenced by the individual’s immune system function and whether appropriate treatment is received. Populations without a history of chickenpox and immunocompromised individuals are at higher risk of contracting the virus and require special attention. Implementing isolation, quarantine, and good hygiene practices during the contagious period is vital to prevent the spread of shingles. Healthcare providers and patients alike should be aware of these factors to ensure proper management and protection of public health. By understanding how long a person with shingles remains contagious, we can take the necessary steps to minimize the impact of this viral infection on individuals and the community.